ACE Inhibitors: How They Lower Blood Pressure and What You Need to Know
When your blood pressure stays too high, your heart and arteries work harder than they should. That’s where ACE inhibitors, a class of medications that block the angiotensin-converting enzyme to relax blood vessels and reduce fluid retention. Also known as angiotensin-converting enzyme inhibitors, they’re one of the most prescribed treatments for high blood pressure, heart failure, and kidney protection in people with diabetes. These drugs don’t just lower numbers—they help prevent long-term damage to your heart, kidneys, and blood vessels.
ACE inhibitors like lisinopril, enalapril, and ramipril work by stopping your body from making too much angiotensin II, a chemical that tightens blood vessels and raises blood pressure. When that enzyme is blocked, your vessels stay relaxed, your kidneys release more sodium and water, and your heart doesn’t have to pump as hard. That’s why they’re often first-line for people with diabetes and kidney disease—they slow down damage better than some other blood pressure pills. But they’re not for everyone. If you’ve had a bad reaction to them before, or if you’re pregnant, your doctor will pick something else. And while they’re generally safe, a dry cough is common enough that many people switch to ARBs, angiotensin receptor blockers, which block the same pathway but at a different point and with fewer side effects like losartan or telmisartan.
What’s interesting is how these drugs connect to other treatments. For example, digoxin, a heart medication used for atrial fibrillation and heart failure, is sometimes used alongside ACE inhibitors when the heart needs extra support. Meanwhile, people on diuretics, like Lasix (furosemide), which help remove excess fluid often get ACE inhibitors too, because together they give better control than either alone. Even though they’re not direct alternatives, they’re frequently part of the same treatment plan. And while some people worry about side effects like dizziness or high potassium, most find them well-tolerated when monitored properly.
You’ll find posts here that compare ACE inhibitors to other blood pressure drugs like telmisartan, explain why some people switch, and even cover what to do if you’re on one and start feeling off. There’s also info on how these drugs interact with other medications, what to watch for, and why your doctor might choose one over another. Whether you’re just starting on an ACE inhibitor, wondering why your doctor picked it, or looking at alternatives, the articles below give you clear, no-fluff answers based on real clinical use—not theory.
Blood Pressure Medications: Types, Side Effects, and Safety
Learn the most common blood pressure medications, their side effects, and safety tips. Understand why certain drugs are chosen based on your health and how to avoid dangerous interactions.
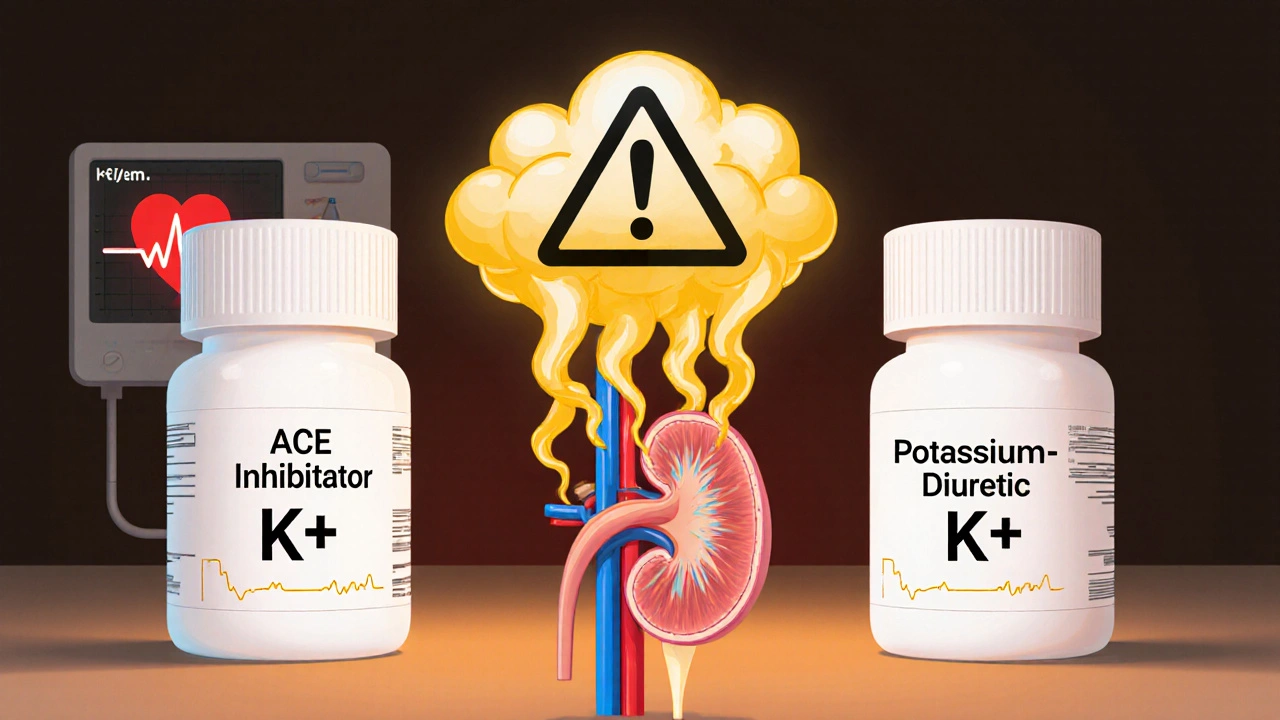
Read moreACE Inhibitors and Potassium-Sparing Diuretics: Understanding the Hyperkalemia Risk
Combining ACE inhibitors and potassium-sparing diuretics can raise potassium to dangerous levels, increasing the risk of heart rhythm problems. Learn how to monitor, manage, and reduce this common but preventable drug interaction.
Read more