High blood pressure doesn’t come with warning signs. You might feel fine, but your arteries are under constant strain. Left untreated, it silently increases your risk of heart attack, stroke, and kidney failure. That’s why millions of people take blood pressure medication every day - not because they’re sick, but because they need to stay well. The problem? Not all meds work the same for everyone, and side effects can make people quit taking them. This isn’t about guessing what works. It’s about knowing exactly what’s in your prescription, why it was chosen, and what to watch for.
How Blood Pressure Medications Work
Blood pressure meds don’t just lower numbers. They target the body’s own systems to reduce pressure in your arteries. Some tell your kidneys to flush out extra salt and water. Others relax blood vessels. Some slow your heart down. Each class works differently, and doctors pick based on your health history, age, race, and other conditions like diabetes or heart failure.
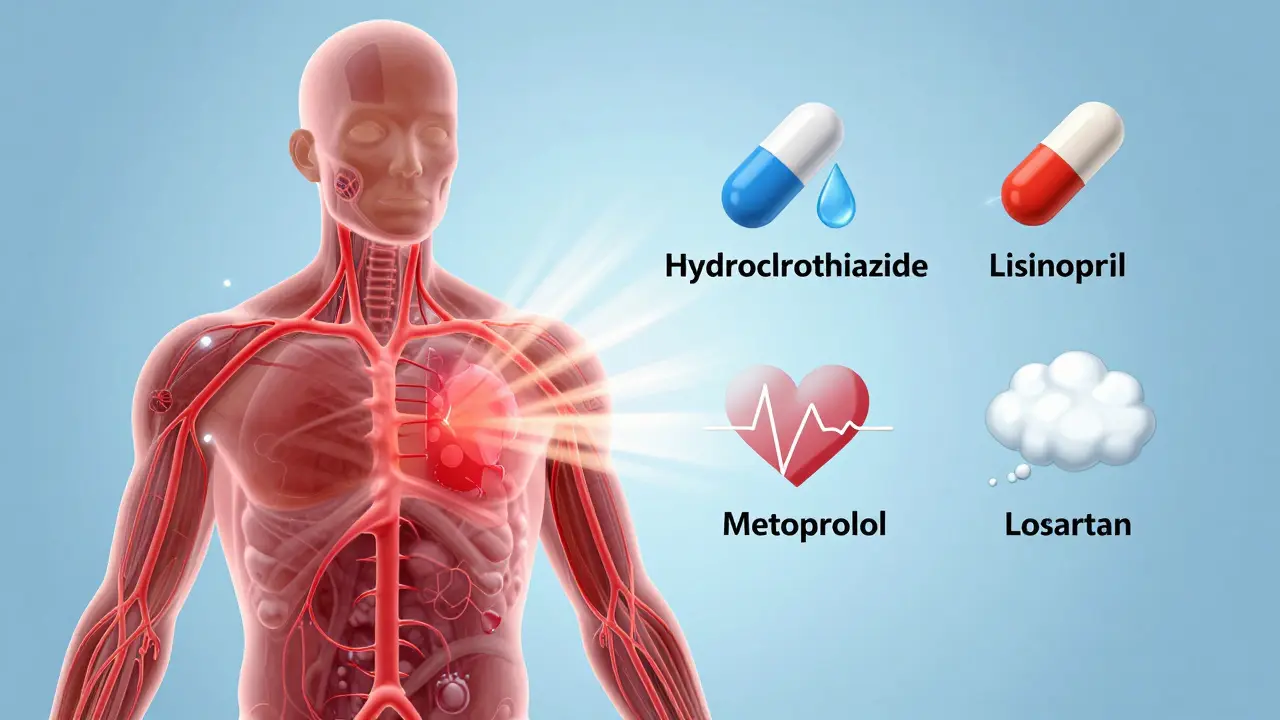
The most common types fall into five main groups. Thiazide diuretics like hydrochlorothiazide are often the first choice. They help your body get rid of extra fluid, which reduces the volume of blood pushing against artery walls. Calcium channel blockers like amlodipine relax the muscles in your arteries, making them wider. ACE inhibitors like lisinopril block a hormone that narrows blood vessels. ARBs like losartan do something similar but block the hormone at a different point. Beta-blockers like metoprolol reduce heart rate and force, lowering the workload on your heart.
There are also less common options - alpha-blockers, vasodilators, and renin inhibitors - usually added when the first-line drugs don’t do enough. The goal isn’t to use the most drugs, but to use the right ones. For most people, one pill isn’t enough. About 70% of patients need two or more medications to reach their target.
Top Five Most Prescribed Blood Pressure Medications
According to prescription data from U.S. pharmacies, these five drugs are the most commonly prescribed:
- Hydrochlorothiazide - a thiazide diuretic, often used alone or paired with other drugs
- Amlodipine - a calcium channel blocker known for long-lasting effects and few daily side effects
- Lisinopril - an ACE inhibitor, widely used for its kidney-protective benefits
- Metoprolol - a beta-blocker, especially common in patients with heart disease
- Losartan - an ARB, often chosen when patients can’t tolerate ACE inhibitors
These aren’t ranked by strength or effectiveness. They’re ranked by how often doctors reach for them first. Hydrochlorothiazide and amlodipine are popular because they’re cheap, effective, and have decades of safety data. Lisinopril is a go-to for people with diabetes or kidney disease. Metoprolol is preferred if you’ve had a heart attack. Losartan is the alternative when a dry cough from lisinopril becomes unbearable.
Common Side Effects by Drug Class
Side effects are the main reason people stop taking their meds. You might feel fine one day, then dizzy the next. Or your ankles swell. Or you can’t sleep. These aren’t random. They’re tied to how the drug works.
Diuretics (like hydrochlorothiazide) make you pee more - that’s the point. But they can also lower potassium too much, leading to muscle cramps or irregular heartbeat. They can trigger gout flare-ups in people who are prone to it.
Calcium channel blockers (like amlodipine) often cause swollen ankles, flushing, or dizziness. Some people get gum swelling, which can look like poor dental hygiene but is actually a drug reaction. Dihydropyridines like amlodipine rarely slow the heart, but non-dihydropyridines like verapamil can cause constipation or slow heart rate.
ACE inhibitors (like lisinopril) are linked to a persistent dry cough in 10-20% of users. It’s not an allergy - it’s a chemical side effect. Some people develop angioedema, a rare but dangerous swelling of the face, lips, or throat. These drugs also raise potassium levels, which can be risky for people with kidney disease.
ARBs (like losartan) avoid the cough but still carry the risk of high potassium and kidney issues. They’re safer for pregnant women than ACE inhibitors - but still not safe at all during pregnancy.
Beta-blockers (like metoprolol) can make you tired, cold, or slow your heart too much. Diabetics need to be careful: these drugs can hide the warning signs of low blood sugar, like shaking or a fast heartbeat.
Some drugs, like carvedilol or labetalol, combine alpha and beta-blocking effects. They’re great for heart failure but can cause dizziness when standing up - a condition called orthostatic hypotension. That’s why older adults often start on lower doses.

Who Should Avoid Certain Blood Pressure Meds?
Not everyone can take every drug. Your health history matters more than your blood pressure number.
If you have asthma or COPD, beta-blockers can tighten your airways and trigger an attack. Doctors avoid them unless you have heart disease and no other options.
If you’re pregnant, ACE inhibitors, ARBs, and direct renin inhibitors are strictly off-limits. They can cause serious birth defects. Methyldopa and labetalol are the standard choices during pregnancy.
If you have severe kidney disease, you need to watch potassium levels closely. ACE inhibitors, ARBs, and potassium-sparing diuretics can push potassium too high, leading to dangerous heart rhythms.
If you’ve had a heart attack with reduced heart function, some calcium channel blockers like diltiazem or verapamil can worsen it. Amlodipine is usually safe, but others aren’t.
And if you take NSAIDs like ibuprofen or naproxen regularly, they can cancel out the effects of ACE inhibitors and diuretics - and even damage your kidneys when combined. Always tell your doctor what over-the-counter meds you’re taking.
Combination Therapy: Why Two Pills Are Often Better Than One
Most people don’t reach their blood pressure goal with just one drug. The 2025 American Heart Association guidelines say that if your blood pressure is 140/90 or higher, you should start with two medications from different classes right away. That’s a big shift from the old way of trying one drug, waiting weeks, then adding another.
Combining drugs lets you use lower doses of each, which reduces side effects. For example, pairing a diuretic with an ACE inhibitor helps balance potassium levels. Amlodipine plus lisinopril works better than either alone. Many pharmacies now sell these combos in a single pill - like lisinopril/hydrochlorothiazide or amlodipine/valsartan - making it easier to remember your doses.
Four-drug combinations are common in resistant hypertension. The standard combo includes a diuretic, a calcium channel blocker, an ACE inhibitor or ARB, and sometimes a beta-blocker or aldosterone blocker like spironolactone. It’s not random. These combinations are backed by clinical trials showing fewer heart attacks and strokes.

Safety Tips: What You Need to Do Every Day
Medication safety isn’t just about what’s in the bottle. It’s about what you do with it.
- Take it at the same time every day. Skipping doses, even once in a while, raises your risk of stroke. Set a phone alarm or use a pill organizer.
- Don’t stop because you feel fine. High blood pressure doesn’t cause symptoms. Feeling good means the medicine is working.
- Watch for swelling, dizziness, or new cough. These aren’t normal. Call your doctor - don’t wait for your next appointment.
- Get your blood and kidney levels checked. Every 3-6 months, especially if you’re on ACE inhibitors, ARBs, or diuretics. Potassium and creatinine levels tell your doctor if the drugs are safe to keep taking.
- Use apps or reminders. Studies show people who use medication apps are 15-20% more likely to stay on track.
One of the biggest mistakes? Assuming side effects will go away. Some do - like dizziness after a few days. Others don’t. If your ankle swelling from amlodipine is still there after a month, ask about switching. If your cough from lisinopril is keeping you up at night, ask for losartan. There are alternatives. You just have to speak up.
What’s Next? Personalized Medicine and New Options
The future of blood pressure treatment isn’t one-size-fits-all. Researchers are studying how your genes affect how you respond to drugs. Some people metabolize beta-blockers slowly - they need lower doses. Others barely respond to ACE inhibitors at all. In the next 5-10 years, genetic testing might help doctors pick your first pill based on your DNA.
New drugs are also on the horizon. Endothelin receptor antagonists and novel vasodilators are being tested for people whose blood pressure won’t budge even with four meds. Digital tools - smart blood pressure cuffs that sync to your phone, AI-driven alerts for missed doses - are becoming part of standard care.
But right now, the best tool you have is knowledge. Know what you’re taking. Know why. Know what to watch for. And never be afraid to ask your doctor: "Is this the right one for me?"
Can I stop taking blood pressure medication if my numbers are normal?
No. Normal blood pressure means the medication is working, not that you no longer need it. Stopping suddenly can cause your pressure to spike, increasing your risk of stroke or heart attack. Some people can reduce or stop meds after major lifestyle changes - like losing weight or cutting salt - but only under a doctor’s supervision. Never stop on your own.
Which blood pressure medication has the least side effects?
There’s no single answer. Amlodipine often has fewer daily side effects than beta-blockers or ACE inhibitors. Thiazide diuretics are well-tolerated by many, but can cause electrolyte issues. ARBs like losartan avoid the dry cough that affects 1 in 5 people on ACE inhibitors. The "least side effects" drug depends on your body, your other conditions, and your genetics. The best choice is the one that works for you without causing problems.
Do blood pressure meds damage your kidneys?
They usually protect them. ACE inhibitors and ARBs are actually used to slow kidney damage in people with diabetes or protein in their urine. But if you’re dehydrated, take NSAIDs like ibuprofen, or have severe kidney disease, these same drugs can cause sudden kidney injury. That’s why regular blood tests are crucial. The risk isn’t from the meds themselves - it’s from how they interact with your body’s condition.
Can I drink alcohol while taking blood pressure medication?
Moderate alcohol - one drink a day for women, two for men - is usually okay. But alcohol lowers blood pressure too, so combining it with meds can make you dizzy or faint, especially when standing up. It can also interfere with how your liver processes the drugs. If you’re on diuretics, alcohol can worsen dehydration. Talk to your doctor about your habits - they need to know to adjust your treatment.
Why do I need to take blood pressure pills for life?
High blood pressure is a chronic condition, like diabetes. The medication doesn’t cure it - it controls it. If you stop, your arteries will tighten again, your heart will work harder, and your risk of complications returns. Some people can reduce or stop meds after losing weight, improving diet, or increasing activity - but that’s rare. For most, lifelong treatment is the safest path to avoid stroke, heart failure, or kidney failure.
Managing blood pressure isn’t about taking pills. It’s about staying in control - of your health, your choices, and your future. The right medication, paired with awareness and communication, can give you decades of life without a heart attack or stroke. But only if you know what you’re taking - and why.

Lisa Cozad
January 10, 2026 AT 01:50Been on amlodipine for 5 years. Swollen ankles? Yeah. But I’d rather have puffy feet than a stroke. Learned to wear compression socks and keep my legs elevated after work. No more dizziness, no more ER visits. This stuff saved my life, even if it’s not pretty.
Also, never thought I’d say this, but I started using a pill organizer app. Game changer. I used to forget half the time. Now I get a little ping at 8 AM like a loyal robot.
Saumya Roy Chaudhuri
January 11, 2026 AT 06:11Let me tell you something about American medicine. You people are addicted to pills. In India, we use neem leaves, garlic, and yoga. My uncle had BP for 30 years, never took a single pill. He walks 10 km every morning, eats no salt, drinks warm water with lemon. You think your amlodipine is magic? It’s just a band-aid on a broken system.
And don’t get me started on those combo pills. Big Pharma’s way of making you dependent. They don’t want you cured-they want you buying.
Ian Cheung
January 12, 2026 AT 14:19Man I used to hate lisinopril like it owed me money. Dry cough so bad I’d wake up choking at 3 AM like a haunted teakettle. Switched to losartan and it was like someone turned off a siren in my throat. No more cough, no more sleepless nights.
Also-side note-never trust a doctor who says ‘just wait, it’ll go away.’ My ankle swelling from amlodipine didn’t go away. It got worse. Took me three visits and a stubborn attitude to get them to swap it out. You’re not crazy if it feels wrong. You’re just not being heard.
And yeah, I use a pill app. I even named it ‘Pill Buddy.’ It’s got a little heart icon. I’m not ashamed.
Also, NSAIDs are the silent BP killers. I used to pop ibuprofen like candy for my back. Now I use heat packs. Best decision ever.
And if you think you can stop meds because your numbers look good? Buddy, that’s like turning off your smoke alarm because the kitchen isn’t on fire right now. The fire’s still in the walls.
Also, potassium levels? Check ‘em. Don’t be that guy who thinks bananas fix everything. They help. But they don’t replace labs.
And if you’re on beta-blockers and you’re diabetic? Please, for the love of all things holy, carry glucose tabs. Your body won’t warn you when it’s crashing. I learned that the hard way.
And yeah, I’m still alive. Still taking pills. Still kicking. And I’m not sorry.
Also, I love my doctor. She listens. That’s rare. Treat her like gold.
Also, if you’re reading this and you’re scared? You’re not alone. We’re all just trying not to die.
Also, I’m not a doctor. But I’ve been on this ride. And I’m still here.
anthony martinez
January 13, 2026 AT 10:19Wow. So we’re just supposed to take five pills a day and call it a lifestyle now? Next thing you know, they’ll be prescribing oxygen for breathing and caffeine for waking up.
And the ‘combination pills’? That’s not medicine, that’s corporate efficiency. One pill to rule them all, right? Convenient. But also kind of terrifying when you think about it.
And don’t even get me started on the ‘use an app’ advice. Yeah, because nothing says ‘healthy life’ like being tracked by an algorithm that wants your data more than your blood pressure.
Also, ‘never stop on your own’-but sure, go ahead and stop if your doctor says so. Trust the system. Totally.
Mario Bros
January 15, 2026 AT 01:46Hey, I was right there with you on the dry cough thing. Lisinopril had me coughing like I was auditioning for a horror movie. Switched to losartan and it was like a weight lifted. No more midnight hacking.
Also, if you’re on diuretics, drink water like it’s your job. I used to skip it because I didn’t want to pee all day. Bad idea. Ended up dizzy at the grocery store. Lesson learned.
And yeah, I take my meds at the same time every day. I even have a little ritual: coffee, then pills, then my dog gives me a look like I’m her favorite human. It’s weird, but it works.
Don’t let side effects scare you off. Talk to your doc. There’s always another option. You’re not broken-you’re just figuring it out.
And hey-you’re doing better than you think. Keep going. 💪
Jake Nunez
January 16, 2026 AT 17:13As someone who grew up in a country where hypertension was treated with herbs and fasting, I’ve seen both sides. The meds work. No doubt. But I’ve also seen people in rural India live into their 90s with no pills, just diet, walking, and community. Maybe the real issue isn’t the drugs-it’s how disconnected we are from our bodies and our food.
Still, I take my amlodipine. Because I’m not trying to be a hero. I’m trying to be here for my kids.
Just saying-don’t forget the simple stuff. Sleep. Walk. Eat real food. Pills help. But they’re not the whole story.
Christine Milne
January 18, 2026 AT 15:28This entire article is a textbook example of pharmaceutical indoctrination. The American Medical Association, in collusion with Big Pharma, has turned a physiological variable into a chronic disease requiring lifelong chemical intervention. Blood pressure is not a disease-it is a measurement. A fluctuating, context-dependent measurement.
And yet, we are told that a reading of 130/80 is a medical emergency requiring lifelong pharmacotherapy. This is not science. This is profit-driven pathology.
Furthermore, the suggestion that patients require multiple medications is not evidence-based-it is a financial incentive disguised as clinical wisdom. The notion that combination pills are ‘convenient’ is a marketing ploy to increase adherence to a regimen that is not only unnecessary for most, but actively harmful.
And the advice to ‘never stop’? That is fear-mongering. Many individuals can normalize their blood pressure through diet, exercise, and stress reduction. But the medical-industrial complex cannot allow that narrative to prevail, because it undermines their revenue model.
Do not be fooled. Question everything. And if you are taking more than one antihypertensive, you are being overmedicated.
Bradford Beardall
January 20, 2026 AT 02:42Just read this whole thing and it’s honestly the most balanced, non-sensational take on BP meds I’ve seen. I’m a nurse, and I see so many patients quit because they don’t understand why they’re on it. This? This is what education should look like.
One thing I’d add-don’t assume your side effects are ‘normal.’ If you’re dizzy every morning, that’s not ‘just part of it.’ That’s your body saying the dose or drug isn’t right. I’ve seen people switch from metoprolol to carvedilol and suddenly have energy again. It’s not magic. It’s matching the drug to the person.
Also, if you’re on lisinopril and you’re African American? Ask about amlodipine instead. Studies show ACE inhibitors are less effective in that group. Most docs don’t know that. You might have to educate them.
And yes, the apps help. I recommend Medisafe. It even tells you if your pill is expired. Weirdly comforting.
And one last thing-don’t feel guilty for needing meds. You’re not weak. You’re smart. You’re managing a silent threat. That’s not failure. That’s strategy.