Vitamin B12 Deficiency: Signs, Causes, and Treatment
When dealing with vitamin B12 deficiency, a condition marked by low levels of the essential nutrient cobalamin in the blood. Also known as cobalamin deficiency, it can trigger fatigue, mood swings, and nerve problems. In plain terms, the body isn’t getting enough of the vitamin it needs to make red blood cells and keep nerves working smoothly. This shortfall can show up as anemia, tingling in the hands and feet, or even memory hiccups. The good news? Spotting the signs early makes fixing the problem a lot easier.
Key Factors Behind Low B12 Levels
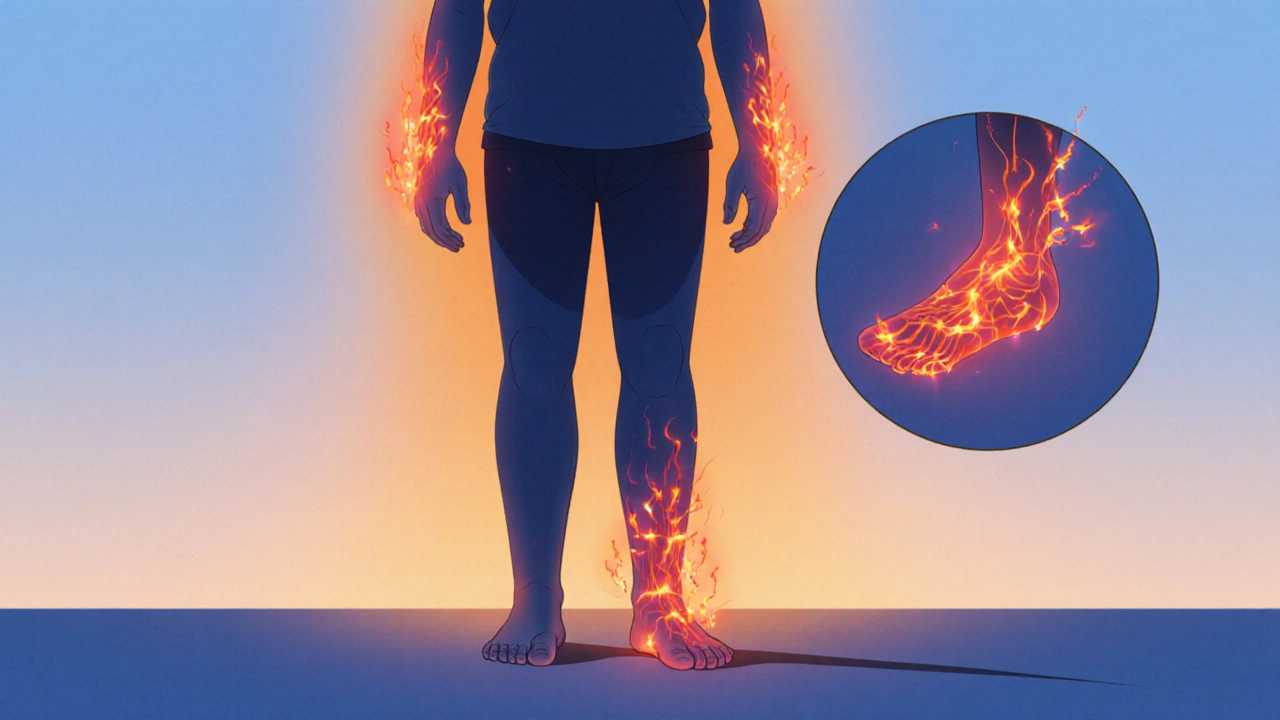
One of the first things to understand is what fuels a proper Vitamin B12, the water‑soluble vitamin also called cobalamin supply. Dietary sources like meat, dairy, and fortified cereals drop the risk of deficiency for most eaters. However, three big roadblocks can still appear. First, poor intake – vegans and strict vegetarians often miss out unless they supplement. Second, absorption issues – conditions such as atrophic gastritis or intestinal surgery can block the vitamin’s journey from gut to bloodstream. Third, autoimmune attack – pernicious anemia, an autoimmune disorder that destroys stomach cells needed to release B12 from food is a classic culprit that silently lowers levels over years. When any of these factors are at play, the body’s nerve fibers bear the brunt, leading to neuropathy, painful or numb sensations caused by damaged peripheral nerves. In short, low B12 encompasses dietary gaps, malabsorption, and autoimmune interference, and it requires a layered diagnostic approach.
How do you know it’s happening? A simple blood test measuring serum B12, methylmalonic acid, and homocysteine can confirm the deficiency and hint at its severity. Doctors often pair labs with a symptom checklist: sluggishness, shortness of breath, swollen tongue, and the classic “pins‑and‑needles” feeling. If you catch these early, treatment can be as straightforward as oral supplements or monthly injections, depending on the root cause. For pernicious anemia, lifelong injections are usually recommended because the stomach can’t absorb pills reliably. For diet‑related gaps, high‑dose oral tablets or fortified foods do the trick. Lifestyle tweaks—adding fish, eggs, or fortified plant milks—support the medical regimen and keep levels stable.
Beyond the medical side, understanding the broader landscape helps you stay proactive. Our collection below brings together practical guides on a range of drugs, supplements, and health conditions that often intersect with B12 issues—think antihistamines that can affect absorption, antibiotics that disturb gut flora, and even mental‑health meds that share side‑effect profiles. Whether you’re hunting for a cheap generic option, comparing brand‑name alternatives, or just curious about how nutrition ties into overall treatment plans, you’ll find clear, side‑by‑side information to guide your choices.
Ready to dive deeper? Browse the articles below to see how specific medications, dietary strategies, and lifestyle changes can support your B12 health, alleviate symptoms, and keep you feeling energetic and focused.
Burning Sensation and Vitamin Deficiency: Causes, Symptoms & Solutions
Explore how vitamin deficiencies-especially B12, B1, and B6-trigger burning sensations, how to diagnose the link, and practical dietary and supplement fixes.
Read more