Vitamin Deficiency Risk Checker
Your Burning Sensation Assessment
Answer a few questions to identify potential vitamin deficiencies causing your symptoms.
Symptom Checklist
Your Lifestyle Factors
Your Risk Assessment
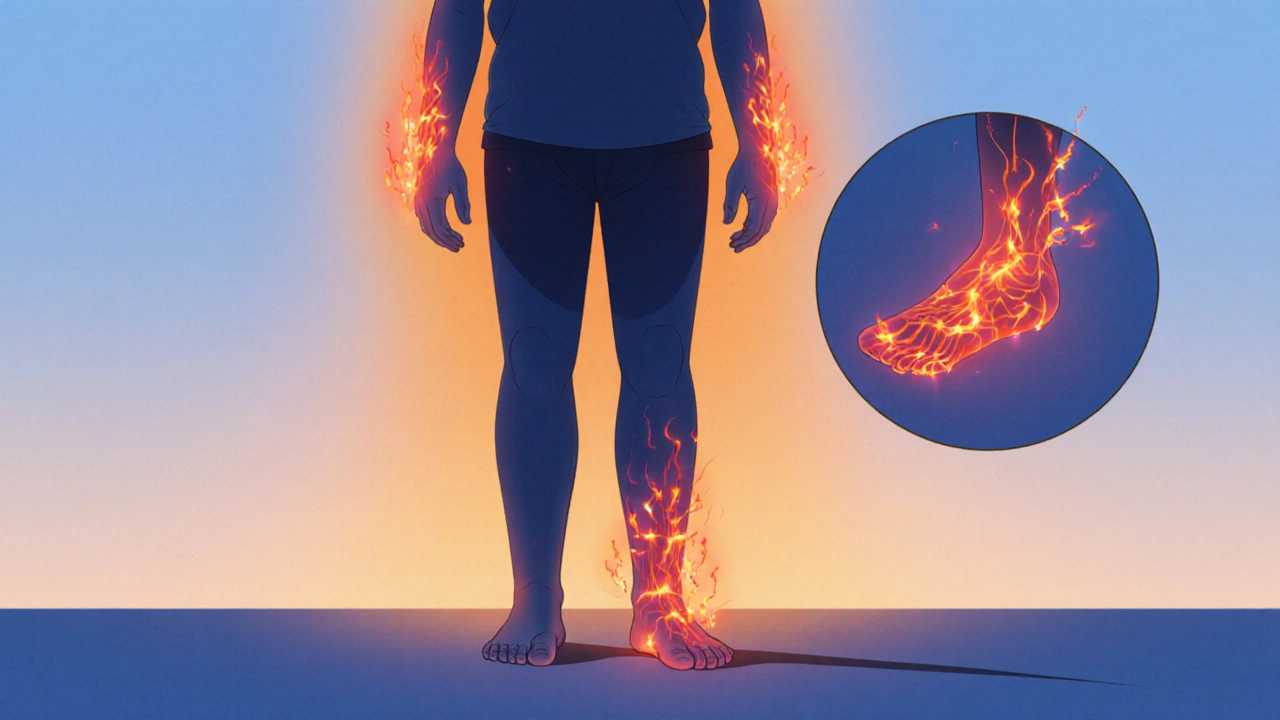
Ever felt a strange, tingling heat on your hands or feet that just won’t quit? That burning sensation could be more than a fleeting itch-it might be a signal that your body’s missing key vitamins. In this guide we’ll walk through why nerves light up when nutrients are low, which deficiencies are the usual suspects, and what you can do to calm the heat.
Key Takeaways
- Burning sensations often stem from nerve irritation caused by vitamin gaps, especially B‑vitamins.
- Vitamin B12, B1 (thiamine), and B6 deficiencies are the most common culprits.
- Lab tests, dietary review, and a quick physical exam can pinpoint the link.
- Targeted supplementation and diet tweaks resolve symptoms in most cases.
- Seek medical attention if the feeling spreads, includes weakness, or is accompanied by numbness.
What Exactly Is a Burning Sensation?
When you hear the term Burning Sensation is the perception of heat, tingling, or pain that feels like a mild fire on the skin, often without any external cause, doctors usually classify it under “paresthesia.” The feeling can appear in one spot (like a fingertip) or run along an entire limb, a pattern known as “burning feet syndrome” when it hits the soles.
These sensations arise when peripheral nerves-the communication lines extending to your hands and feet-become irritated or damaged. The irritation can be electrical, chemical, or metabolic. While diabetes, infections, and toxin exposure are well‑known triggers, nutrient shortfalls are sneaky, often overlooked contributors.
How Vitamins Keep Nerves Healthy
Vitamins are more than just “good for you” labels; they serve as co‑factors in biochemical pathways that maintain the myelin sheath-the protective coating around nerve fibers. Without adequate support, the sheath degrades, leading to erratic firing and the uncomfortable heat you feel.
Key roles:
- Vitamin B12 (cobalamin) is essential for DNA synthesis and myelin production. A deficiency stalls myelin formation, causing demyelination.
- Vitamin B1 (thiamine) drives carbohydrate metabolism, supplying energy to nerve cells.
- Vitamin B6 (pyridoxine) helps synthesize neurotransmitters like serotonin and GABA, balancing nerve signaling.
- Vitamin D influences calcium channels that affect nerve excitability.
- Vitamin E acts as an antioxidant, shielding nerve membranes from oxidative damage.
When any of these vitamins dip below optimal levels, nerves can misfire, producing that classic burning feeling.

Common Vitamin Deficiencies Linked to Burning Sensation
| Vitamin | Primary Deficiency Symptoms | Typical Burning‑Related Signs |
|---|---|---|
| B12 | Fatigue, anemia, glossitis | Numbness, tingling, burning feet/hands |
| B1 (Thiamine) | Beriberi, heart failure, confusion | Peripheral neuropathy, burning in legs |
| B6 (Pyridoxine) | Seizures, dermatitis, anemia | Sensory neuropathy, burning wrists |
| D | Bone pain, muscle weakness | Hyperexcitability, tingling, occasional burning |
| E | Muscle weakness, vision problems | Peripheral nerve degeneration, burning sensations |
Among these, B12 deficiency tops the list for adult‑onset burning sensations, especially in vegans, older adults, and people on proton‑pump inhibitors that reduce stomach acid.
Diagnosing the Vitamin‑Burning Link
- Medical History Review: Doctors ask about diet (vegan, low‑meat, high‑processed), medication use, and alcohol intake.
- Physical Examination: A quick reflex test and skin exam can reveal loss of sensation or hyper‑sensitivity.
- Blood Tests: Serum B12, folate, methylmalonic acid, homocysteine, and levels of B1, B6, D, and E give a clear picture.
- Neurological Tests: Nerve conduction studies rule out other causes like diabetic neuropathy.
- Dietary Assessment: A dietitian may use a food‑frequency questionnaire to spot gaps.
If labs confirm low vitamin levels, the link to the burning feeling becomes much clearer.
Managing Symptoms Through Diet and Supplements
Addressing the root cause has two fronts: what you eat and what you add on top.
- Boost B12: Include meat, fish, dairy, or fortified plant milks. For vegans, a daily cyanocobalamin supplement (25‑100 µg) works well.
- Increase B1: Whole grains, legumes, nuts, and pork are rich sources. A supplement of 50‑100 mg per day can reverse early neuropathy.
- Support B6: Bananas, chickpeas, and potatoes provide pyridoxine. Avoid megadoses (>200 mg) as they can paradoxically cause neuropathy.
- Vitamin D: Sun exposure (10‑15 minutes a few times a week) plus fortified foods or 800‑1000 IU daily if blood levels are <20 ng/mL.
- Vitamin E: Almonds, sunflower seeds, and spinach. A supplement of 100‑200 IU can help when deficiency is proven.
Most patients notice a reduction in burning within 2-4 weeks of correcting the deficiency. It’s crucial to repeat blood tests after 8-12 weeks to confirm levels have normalized.

When to Seek Medical Attention
If the sensation spreads rapidly, is accompanied by muscle weakness, loss of balance, or visual changes, it may signal a more serious neurological issue. Similarly, if you have a chronic condition like diabetes, a new burning feeling warrants a prompt check‑up to rule out overlapping neuropathies.
Red‑flag symptoms:
- Sudden onset of severe pain.
- Persistent numbness that progresses proximally.
- Difficulty walking or using hands for fine tasks.
- Unexplained weight loss or chronic fatigue.
In such cases, a physician might order imaging (MRI) or referrals to a neurologist for deeper evaluation.
Quick Checklist to Prevent Burning Sensations
- Eat a balanced diet with animal proteins or fortified alternatives.
- Limit alcohol to moderate levels; excessive intake depletes B‑vitamins.
- Check medication side‑effects-some antacids and metformin lower B12 absorption.
- Get yearly blood work if you’re over 60, vegan, or have gastrointestinal disorders.
- Stay active; regular exercise improves circulation to peripheral nerves.
Frequently Asked Questions
Can a burning sensation be a sign of something other than vitamin deficiency?
Yes. Conditions like diabetes, shingles, peripheral artery disease, and certain medications can also cause burning sensations. A thorough medical evaluation is needed to rule out these causes.
How quickly do symptoms improve after starting supplements?
Most people report noticeable relief within 2-4 weeks, but total recovery may take up to 3 months, especially if nerve damage was moderate.
Is it safe to self‑diagnose a vitamin deficiency based on a burning feeling?
Self‑diagnosis is risky. While diet clues help, blood tests provide objective confirmation before starting high‑dose supplements.
Do vegetarians need to take B12 supplements?
Yes, unless they regularly consume B12‑fortified foods. A daily 25‑100µg cyanocobalamin supplement is recommended.
Can too much vitamin B6 cause burning sensations?
Paradoxically, very high doses of B6 (>200mg/day) can lead to peripheral neuropathy, which feels like burning. Stick to recommended amounts.

Frank Diaz
October 17, 2025 AT 17:23The heat that creeps along a fingertip is not merely a nuisance; it is the body’s silent testimony to a biochemical imbalance. When myelin loses its protective sheath, electrical storms erupt, and the nervous system screams in fire. Deficiencies in B‑vitamins act as the silent saboteurs, stripping nerves of the co‑factors they need to function. Consider the paradox of modern diets: abundant calories yet woefully lacking in micronutrients. Thus the burning sensation becomes a moral indictment of our nutritional neglect.
Mary Davies
October 22, 2025 AT 08:30In the quiet of night I once felt my palms ignite, a drama only the nerves could stage. The sensation lingered like a lingering spotlight, refusing to dim as I searched for a cause. Realizing it was linked to a lack of B12 felt like uncovering a hidden script in my own body. It taught me that even the smallest nutrient can wield the power of a thunderclap.
Valerie Vanderghote
October 25, 2025 AT 19:50When you sit at a kitchen table and stare at a half‑eaten plate of processed snacks, you may think you are simply indulging in convenience, but the quiet betrayal of your nervous system is already at work, threading its way through the synaptic gaps like an unseen thief in the night, stealing the essential B‑vitamins that keep the myelin sheath thick and resilient, and without those guardians, the nerves begin to whisper, then shout, in the language of fire that we mistake for a random tingling. The first time I experienced that burning feeling in my left foot, I dismissed it as a fleeting footache from a too‑tight shoe, but the pain persisted, spreading up the calf and then curling around my toes like a living ember, refusing to be ignored. I consulted a weary physician who skimmed through my medical history, noted my vegan diet, and ordered a battery of blood tests that revealed a stark deficiency in cobalamin, a vitamin that many of us consider optional because we trust fortified cereals to fill the gap. The doctor prescribed a high‑dose B12 injection, and within days the fire receded, leaving behind a calm that felt almost foreign after weeks of internal combustion. Yet the story does not end with a simple injection; it is a cascade of lifestyle choices, each linked to the subtle erosion of nerve health, from chronic stress that depletes magnesium, to excessive coffee that impairs B6 absorption, to sedentary habits that limit sunlight and thus vitamin D synthesis, each factor a thread in the tapestry of neuropathy. Moreover, the hidden culprits-certain medications like proton‑pump inhibitors-silently lower stomach acidity, preventing the release of bound B12 from food, turning well‑intentioned meals into nutritional voids. I remember reading a study that connected prolonged use of these drugs to a 30 percent increase in peripheral neuropathy cases, a statistic that feels like a warning sign flashing across a highway at night. Adding to the complexity, genetic variations in the MTHFR enzyme can blunt the conversion of folate into its active form, compounding the deficiency and amplifying the burning sensation. In my own journey, I discovered that supplementing with methylated forms of B12 and B9, alongside a balanced intake of riboflavin and pyridoxine, created a synergistic shield around my nerve fibers, restoring their ability to conduct signals without the erratic sparks of fire. The diet I now follow is intentional: leafy greens for folate, fortified plant milks for B12, whole grains for thiamine, and occasional fatty fish for the rare dopamine boost, all punctuated by sunlight walks that coax vitamin D into my bloodstream. It is a regimen that requires vigilance, because the body does not send a polite reminder when the reserves dwindle; it merely ignites the nerves, demanding attention. As I reflect, I realize that the burning sensation is not merely a symptom but a messenger, urging us to reevaluate the foundations of our nutrition, the hidden chemicals we ingest, and the lifestyle choices that either fan the flames or douse them with care. If you find yourself plagued by that inexplicable heat, consider the full spectrum of possible deficiencies, not just the headline B‑vitamins, and remember that the path to relief often begins with a simple blood test and ends with a comprehensive, personalized plan that respects the intricate chemistry of your own biology.
Emily (Emma) Majerus
October 29, 2025 AT 20:03Got ur point, just pop a B12 supplement now.
Virginia Dominguez Gonzales
November 1, 2025 AT 03:37That simple step can feel like a sunrise after a night of endless fire, illuminating the path to comfort and health. Remember, consistency beats intensity; a daily B12 dose builds a fortress around your nerves. You’ve got this, and every small choice adds up to real relief.
Carissa Padilha
November 4, 2025 AT 14:57The whole emphasis on “just take a vitamin” is a neat distraction engineered by the supplement industry to keep us buying endless pills while the real issue-industrial food manipulation-remains hidden. They’ll never mention how modern agriculture depletes soil of micronutrients, turning our produce into nutritional ghosts. By focusing on a single deficiency, they steer the conversation away from the systemic problem of a diet stripped of natural diversity. It’s a classic divide‑and‑conquer tactic, letting us think we’re fixing a problem while the larger illness persists. Keep questioning the narrative, and look beyond the label.
Richard O'Callaghan
November 7, 2025 AT 12:23i think you r right the food indstry does a lot but we still need the vit B12 for nerves it is real
Alexis Howard
November 10, 2025 AT 23:43maybe supplements aren't even needed
Kevin Adams
November 13, 2025 AT 07:17Ah, the audacity of those who claim we can merely forgo the very building blocks of our neural architecture!-What a reckless proclamation, shouted from the rooftops of complacency!-Do you not see that B‑vitamins are the silent architects of our sensory world, laying down the scaffolding upon which every tingling whisper depends?-To deny them is to invite chaos into the very marrow of our being!-Let the fire burn, yes, but let it be the fire of awareness, not the flame of ignorance!-
Russell Abelido
November 16, 2025 AT 18:37I feel your frustration, and I’ve walked that same scorching path; the burning feeling can feel like an unwelcome spotlight on your body 😔. It’s amazing how a simple B12 boost can turn that blaze into a gentle glow, reminding us that our bodies are wiser than we sometimes give them credit for. Keep listening to those signals, they’re trying to guide you toward balance.
Steve Holmes
November 19, 2025 AT 16:03Absolutely, Russell, your insight resonates deeply, and it highlights the importance of not just treating symptoms, but also investigating the underlying nutritional landscape, especially when a vitamin deficiency can masquerade as a mysterious fire, igniting sensations that are both unsettling and instructive, and when we address the root cause with targeted supplementation, dietary adjustments, and perhaps even lifestyle changes, we often witness a remarkable transformation that restores comfort and stability to the nervous system.
Tom Green
November 23, 2025 AT 03:23Let’s remember that each person's journey with nutrient deficiencies is unique, and fostering a supportive community can make the path to recovery less daunting. Sharing experiences, lab results, and dietary tips empowers everyone to make informed decisions.
Emily Rankin
November 25, 2025 AT 10:57Indeed, the collective wisdom we build becomes a lighthouse amid the fog of confusion, guiding us toward brighter health horizons. When we combine scientific knowledge with hopeful perseverance, even the most stubborn burning sensations can be soothed. Your encouragement lifts spirits, reminding us that every step forward, no matter how small, is a victory worth celebrating.
Rebecca Mitchell
November 28, 2025 AT 08:23yes shared knowledge heals