Overactive Bladder: Causes, Treatments & Everyday Tips
When dealing with Overactive Bladder, a condition marked by sudden urges, frequent bathroom visits, and occasional leakage. Also known as urge incontinence, it touches millions of lives and can throw off work, sleep, and social plans. Overactive bladder isn’t just a nuisance; it signals that the bladder’s muscle control system is out of balance, often because nerves overreact to normal filling. Understanding this imbalance is the first step toward relief.
Key Strategies to Manage Overactive Bladder
Medical therapy usually starts with anticholinergic medication, drugs that calm the bladder’s detrusor muscle to reduce urgency spikes. These agents directly influence muscle activity, lowering the frequency of sudden urges. For people who can’t tolerate meds or prefer non‑drug routes, pelvic floor therapy, targeted exercises that strengthen the muscles supporting the bladder and urethra provides a hands‑on way to boost control. Meanwhile, bladder training, a structured schedule that gradually extends the interval between voids teaches the nervous system to tolerate larger volumes before signaling. Together, these approaches form a trio: medication calms the muscle, therapy strengthens the support, and training rewires the timing.
Beyond the core trio, lifestyle tweaks play a big role. Caffeine, alcohol, and spicy foods can irritate the bladder lining, making urgency worse. Hydration matters too—drinking enough water prevents concentrated urine, but spreading fluid intake throughout the day avoids overloading the bladder at once. Simple habits like a timed bathroom routine, double‑voiding (urinating twice in a row), and using a bladder diary to spot patterns can pinpoint triggers. When combined with pelvic floor exercises, these habits often reduce leaks enough to skip medication altogether.
In many cases, a multidisciplinary plan yields the best results. Urologists, primary care doctors, physical therapists, and dietitians each bring a piece of the puzzle. For example, a therapist might teach the correct contract‑relax cycle for pelvic muscles, while a doctor adjusts dosages of anticholinergics or introduces newer agents like beta‑3 agonists if needed. This collaborative model respects that overactive bladder encompasses nerve signaling, muscle tone, and daily habits—all of which need coordinated attention.
Understanding that overactive bladder is manageable rather than inevitable opens the door to real improvement. Below you’ll discover articles that dive deeper into each of these topics—medication choices, step‑by‑step pelvic floor routines, effective bladder‑training schedules, and everyday lifestyle hacks—to help you take charge of your bladder health.
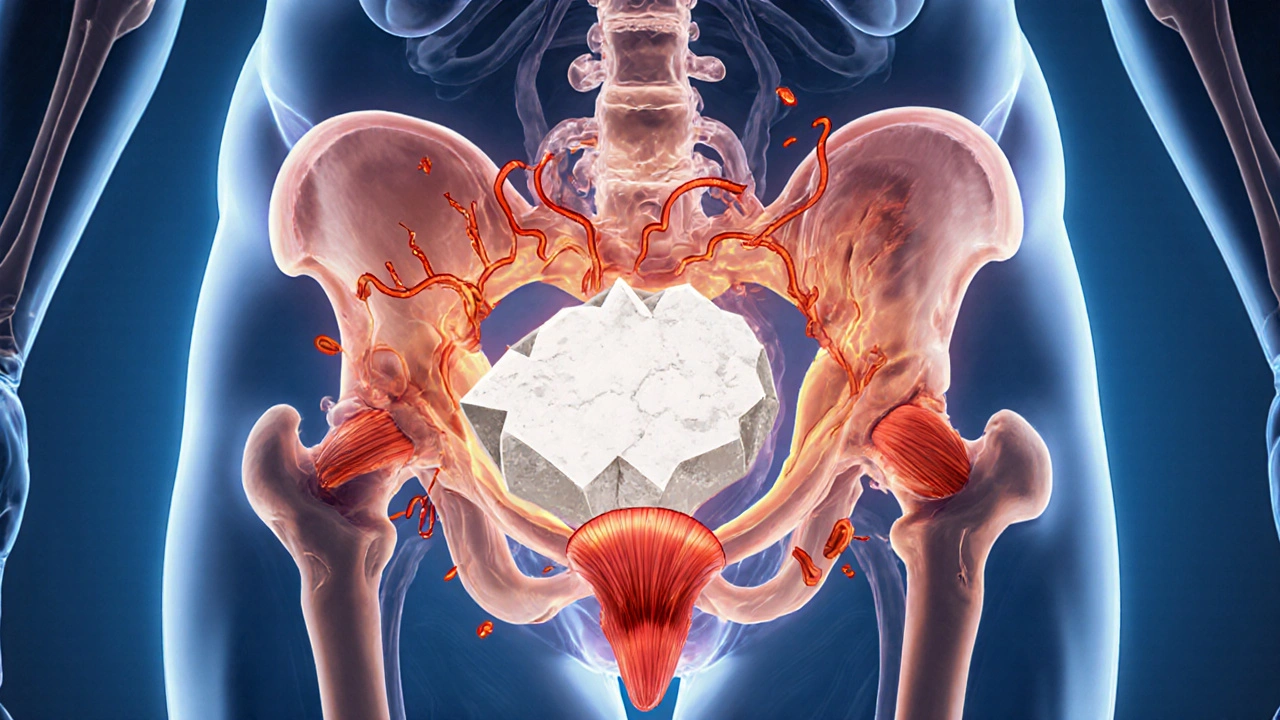
Bladder Stones and Urinary Tract Muscle Spasms: Causes, Connection, and Relief
Explore how bladder stones trigger urinary tract muscle spasms, their shared risk factors, diagnosis, and effective treatments to prevent pain and recurrence.
Read more