Bladder Stone Prevention Hydration Calculator
Stay Hydrated to Prevent Bladder Stones
Proper hydration is one of the most effective ways to prevent bladder stones and reduce urinary tract spasms. The article discusses how drinking at least 2.5 liters of water daily helps flush out minerals before they can form stones.
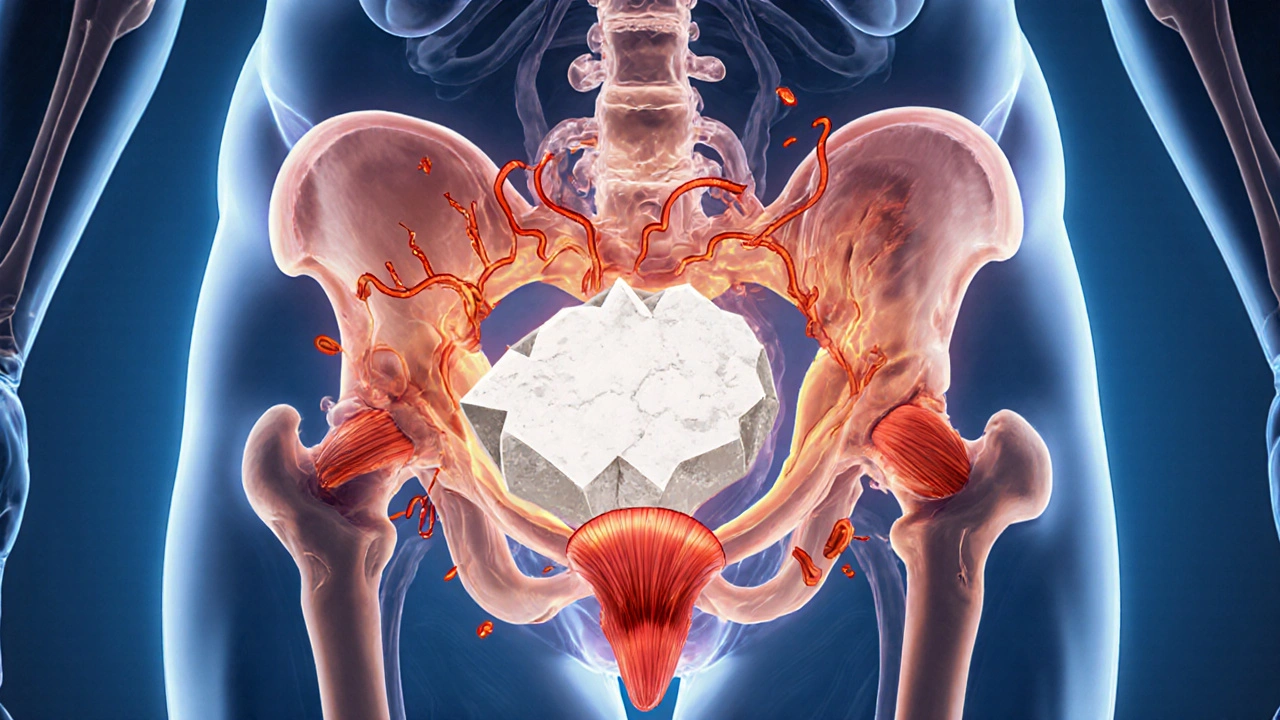
When a bladder stone is a hard mineral deposit that forms inside the bladder, it can do more than just cause pain-it often triggers painful muscle spasms throughout the urinary tract.
What Are Bladder Stones?
Bladder stones, also called vesical calculi, are solid masses made of minerals such as calcium oxalate, uric acid, or struvite. They develop when urine becomes supersaturated with these substances and the bladder cannot flush them out. Unlike kidney stones, which typically form in the renal pelvicalyceal system, bladder stones stay in the lower urinary tract and may grow larger over time.
Common symptoms include frequent urination, a burning sensation, cloudy urine, and occasional blood in the urine (hematuria). If a stone is large enough, it can block the urethra, leading to acute urinary retention-a medical emergency.
What Triggers Muscle Spasms in the Urinary Tract?
Muscle spasms, medically termed detrusor overactivity or urethral spasm, occur when the smooth muscle lining the bladder and urethra contracts involuntarily. The detrusor muscle normally relaxes to store urine and contracts during voiding. When the coordination fails, you feel urgency, leakage, or painful cramping.
Key contributors to these spasms are:
- Infection: Bacterial cystitis irritates the bladder wall.
- Neurological irritation: Nerve signals from the spinal cord become erratic after trauma or disease.
- Mechanical irritation: Any foreign body-like a bladder stone-can press on the urothelium and trigger reflex contractions.
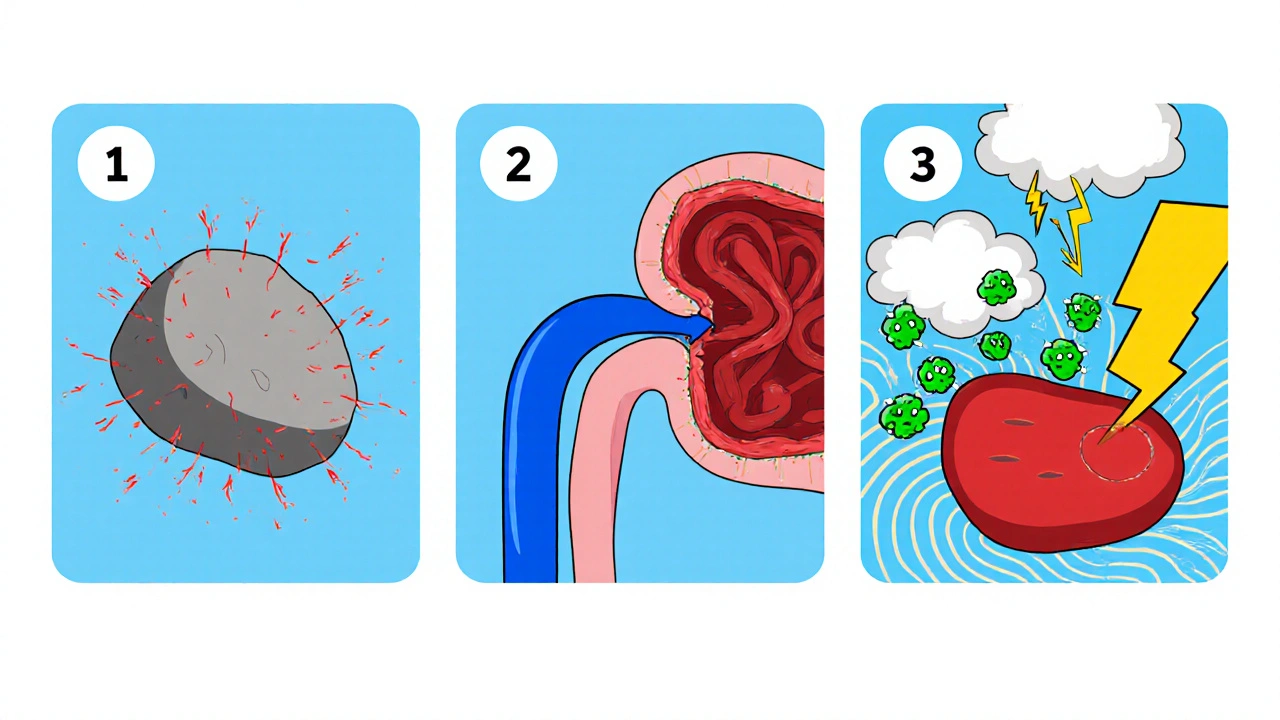
How Bladder Stones Can Set Off Urinary Tract Spasms
The link between stones and spasms is primarily mechanical and chemical:
- Direct Physical Irritation: As a stone rolls around, it scrapes the bladder lining, causing micro‑abrasions. Those tiny wounds release inflammatory mediators (histamine, prostaglandins) that sensitize nearby nerves.
- Obstruction and Pressure: When a stone partially blocks the urethra, urine backs up, increasing intravesical pressure. The bladder responds by sending stronger, more frequent contraction signals-exactly what feels like a spasm.
- Infection Cascade: Stagnant urine around a stone becomes a breeding ground for bacteria. An infection further inflames the wall, amplifying nerve irritation and making spasms more frequent.
Studies from urology departments in 2023 show that up to 42 % of patients presenting with bladder stones also report acute episodes of detrusor overactivity.
Risk Factors and Prevention Strategies
Understanding why stones form helps you break the cycle:
- Dehydration: Low fluid intake concentrates urine, raising the chance of mineral precipitation.
- Dietary Oxalates: Foods like spinach, nuts, and tea increase calcium oxalate levels.
- Chronic Urinary Tract Infections (UTIs): Repeated infections promote struvite stone formation.
- Bladder Outlet Obstruction: Conditions such as benign prostatic hyperplasia (BPH) or urethral strictures limit urine flow, encouraging stone buildup.
- Metabolic Disorders: Gout, hyperparathyroidism, and certain renal tubular defects raise uric acid or calcium concentrations.
Prevention tips:
- Drink at least 2.5 liters of water daily; spread intake throughout the day.
- Limit high‑oxalate foods if you have a known calcium oxalate tendency.
- Manage underlying conditions-control blood sugar, treat gout, and monitor calcium levels.
- Practice good bladder hygiene: fully empty the bladder when you can, and avoid holding urine for long periods.
Diagnosing Stones and Muscle Spasms
Accurate diagnosis starts with a thorough history and physical exam, followed by imaging and lab tests:
| Test | Purpose | Typical Findings |
|---|---|---|
| Ultrasound | Detect stone size & location | Echogenic mass with posterior shadowing |
| CT Scan (non‑contrast) | Gold standard for stone composition | Hyperdense calculi, precise measurements |
| Urinalysis | Identify infection, crystal type | Positive nitrite, leukocytes, crystal morphology |
| Urodynamics | Assess bladder muscle activity | Detrusor overactivity patterns |
When a stone is confirmed, the urologist will also evaluate for concurrent spasms using urodynamic studies. This two‑pronged approach ensures both problems are addressed simultaneously.
Treatment Options for Stones and Spasms
Therapy focuses on removing the stone, relieving irritation, and calming the overactive muscles.
Stone Removal Techniques
- Cystolitholapaxy: A small endoscope fragments the stone with a laser, allowing the pieces to be flushed out.
- Transurethral Cystolithotomy: For very large stones, the surgeon makes a tiny incision through the urethra and extracts the stone whole.
- Extracorporeal Shock Wave Lithotripsy (ESWL): Shock waves break the stone into passable fragments; more common for kidney stones but occasionally used for bladder stones.
Managing Muscle Spasms
- Alpha‑blockers (e.g., tamsulosin) relax smooth muscle in the bladder neck and urethra, reducing spasm frequency.
- Antimuscarinic agents (e.g., oxybutynin) dampen detrusor overactivity, easing urgency.
- Behavioral therapy: Timed voiding and bladder training help retrain the nervous system.
- Pelvic floor physical therapy: Targeted stretches release muscle tension that can exacerbate spasms.
In many cases, removing the stone alone resolves the spasm cycle, but adjunct medication speeds recovery and prevents recurrence.
Lifestyle Adjustments to Keep Both Problems at Bay
Long‑term success hinges on daily habits:
- Hydration timing: Aim for a urine output of at least 1.5 L per day; sip water throughout the day rather than gulping a few large volumes.
- Balanced diet: Include citrus fruits (which contain citrate-a natural stone inhibitor) while moderating high‑oxalate foods.
- Regular voiding schedule: Empty the bladder every 3‑4 hours, especially after fluid intake.
- Avoid bladder irritants: Limit caffeine, alcohol, and spicy foods that can provoke muscle contraction.
- Follow‑up imaging: A repeat ultrasound 3 months after stone removal confirms no residual fragments.
Adopting these practices reduces both stone formation risk and the likelihood of recurrent muscle spasms.
Frequently Asked Questions
Can bladder stones cause permanent damage to the bladder?
If left untreated, large stones can erode the bladder lining, leading to scarring (fibrosis) and reduced bladder capacity. Prompt removal usually prevents lasting damage.
What’s the difference between bladder stones and kidney stones?
Kidney stones form in the renal pelvis and travel down the ureter, often causing flank pain. Bladder stones stay in the bladder, producing urinary frequency, urgency, and sometimes spasms.
Do overactive bladder medications help with stone‑induced spasms?
Yes. Antimuscarinic drugs calm the detrusor muscle, easing urgency that may be triggered by stone irritation. They are often prescribed alongside stone removal.
How soon after stone removal should I expect muscle spasms to stop?
Most patients notice a reduction within a week, though lingering inflammation can keep spasms going for up to a month. Follow‑up urodynamic testing can confirm resolution.
Is surgery the only way to get rid of bladder stones?
Small stones (< 5 mm) may pass spontaneously with high fluid intake and a mild diuretic regimen. Larger stones generally require endoscopic removal or lithotripsy.

Mike Peuerböck
October 23, 2025 AT 19:25Bladder stones are not just a nuisance they can trigger a cascade of uncomfortable events. When a stone tumbles in the bladder it irritates the lining creating micro‑abrasions. Those tiny wounds release inflammatory mediators that sensitize the surrounding nerves. The sensitized nerves then fire off signals that the brain reads as urgency and cramping. In addition the stone can partially block the urethra raising intravesical pressure. The bladder reacts by contracting more forcefully attempting to expel the obstruction. This over‑active response manifests as detrusor overactivity or spasms. If bacteria colonize the stagnant urine surrounding the stone the inflammation worsens. The infection adds histamine and prostaglandins to the mix amplifying the neural irritation. Patients often report a burning sensation during voiding accompanied by frequent urges. Imaging such as ultrasound or non‑contrast CT can reveal the size and location of the stone. Urodynamic studies are useful to quantify the frequency and amplitude of muscle spasms. Treatment normally begins with stone removal through cystolitholapaxy or laser fragmentation. Once the irritant is gone the bladder muscle usually settles back to normal tone. Adjunct medication like antimuscarinics can speed recovery especially if spasms persist. Long‑term prevention hinges on staying well hydrated and managing metabolic risk factors.
Celeste Flynn
October 25, 2025 AT 01:53Great summary and the emphasis on fluid intake is spot on. Adding citrus fruits like lemons can boost citrate levels which naturally inhibit stone formation. For patients with recurrent infections a low‑dose prophylactic antibiotic may reduce the bacterial load and therefore inflammation. It’s also worth noting that pelvic floor physical therapy can help modulate detrusor overactivity after stone removal. Monitoring urine pH can guide dietary adjustments to prevent specific stone types.
Simon Waters
October 26, 2025 AT 07:26Everything they say about staying hydrated is a ploy by the water industry to keep us drinking their chemically treated supply.
CASEY PERRY
October 26, 2025 AT 10:13From a urological perspective the pathophysiology involves mechanotransduction pathways mediated by TRPV1 receptors leading to heightened afferent signaling.
Naomi Shimberg
October 27, 2025 AT 16:46While the prevailing narrative glorifies hydration, one must consider the osmotic burden imposed by excessive water consumption on renal handling of electrolytes.
Vikas Kumar
October 27, 2025 AT 19:33Our nation’s doctors ignore how western diets loaded with processed foods are the real culprits behind these stones and the accompanying spasms.
kenny lastimosa
October 27, 2025 AT 22:20It is interesting to contemplate whether the bladder, in its quest for equilibrium, merely reflects a deeper discord between bodily systems and external influences.
Shan Reddy
October 29, 2025 AT 04:53Totally agree that drinking enough water is key but don’t forget to move around – a short walk can help the bladder empty more completely.
Heather ehlschide
October 29, 2025 AT 07:40For anyone dealing with post‑procedural spasms, a gradual bladder training schedule starting with timed voids every four hours can be very effective.
Kajal Gupta
October 29, 2025 AT 10:26Interesting read.