Medicare Part B Biosimilars: What You Need to Know About Cost-Saving Biologic Alternatives
When you hear Medicare Part B biosimilars, biologic drugs that are highly similar to already-approved brand-name biologics and covered under Medicare Part B for outpatient use. Also known as biologic generics, they’re not exact copies like traditional generics—they’re complex molecules made from living cells, but they work the same way and cost far less. This matters because biologics for conditions like rheumatoid arthritis, cancer, and diabetes can cost over $20,000 a year. Biosimilars cut that price by 15% to 35%, and Medicare Part B covers them just like the original drugs—meaning you pay the same coinsurance, usually 20% after your deductible.
But here’s the catch: not all providers know how to explain the difference between a biosimilar and a generic. A biosimilar, a biologic drug approved by the FDA after proving it has no clinically meaningful differences from its reference product isn’t like a pill version of a brand drug. It’s made in a living system—cells, proteins, fermentation tanks—so tiny variations happen. That’s why the FDA requires extensive testing. Still, studies show biosimilars are just as safe and effective. For example, biosimilars for adalimumab (Humira) and bevacizumab (Avastin) have been used safely by millions since 2016. And when Medicare Part B pays for them, it saves billions that could help fund other care.
Another key player here is the biologic, a complex medication derived from living organisms, used to treat chronic diseases like autoimmune disorders and cancer. These aren’t made in a lab with chemicals—they’re grown in bioreactors. That’s why they’re expensive and hard to copy exactly. Biosimilars bridge the gap: they give patients access to life-changing treatments without the sky-high price tag. And because Medicare Part B covers them under the same rules as the original biologics, switching doesn’t mean losing coverage or facing surprise bills.
Many people still think biosimilars are risky or "second-rate." But the truth? Doctors who use them report fewer side effects than expected, and patients often save hundreds a month. The real barrier isn’t safety—it’s confusion. Pharmacists, nurses, and even some doctors still hesitate to recommend them because they’re not taught how to explain them clearly. That’s changing fast. With more biosimilars approved each year, and Medicare pushing for cost control, you’re more likely to be offered one soon.
What you’ll find in the posts below are real, practical guides on how biosimilars fit into your care. From how to talk to your doctor about switching from a brand biologic, to why some patients still prefer the original, to how Medicare handles payment and prior authorization. You’ll also see how biosimilars connect to broader topics like generic drug trust, medication safety, and managing multiple prescriptions. No fluff. Just what you need to know to make smart choices—whether you’re on insulin, a cancer drug, or a treatment for arthritis.
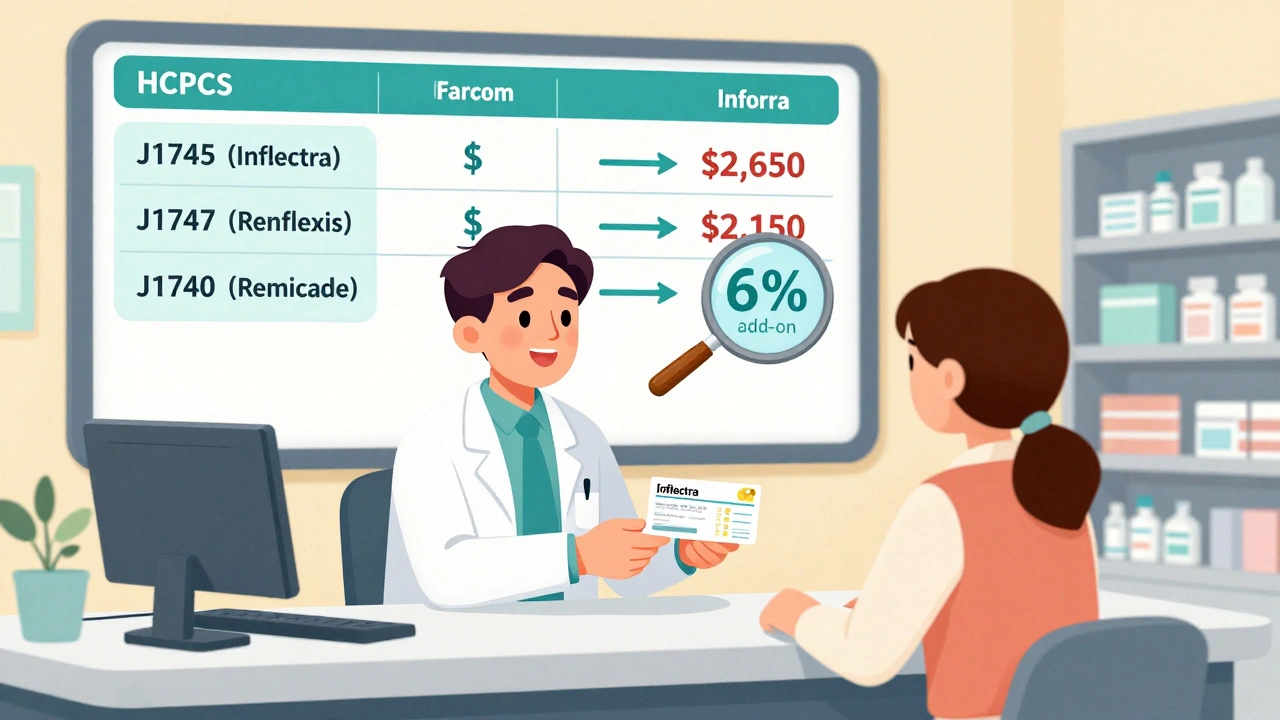
Reimbursement and Coding for Biosimilars: How Billing Works Under Medicare Part B
Learn how biosimilars are billed under Medicare Part B, including HCPCS coding, reimbursement calculations, the JZ modifier, and why adoption remains low despite cost savings. Understand the system providers use and how it affects patient access.
Read more