HCPCS Codes for Biosimilars: What You Need to Know
When you hear HCPCS codes for biosimilars, unique identifiers used by Medicare and insurers to track and pay for biological drugs that are highly similar to brand-name biologics. Also known as healthcare common procedure coding system codes, they’re not just paperwork—they’re the key to getting affordable treatments approved and covered. Unlike regular generics, biosimilars aren’t exact copies. They’re complex, made from living cells, and require special coding to tell them apart from the original biologic. Without the right HCPCS code, a pharmacy might not get paid, and your prescription could be delayed—or denied.
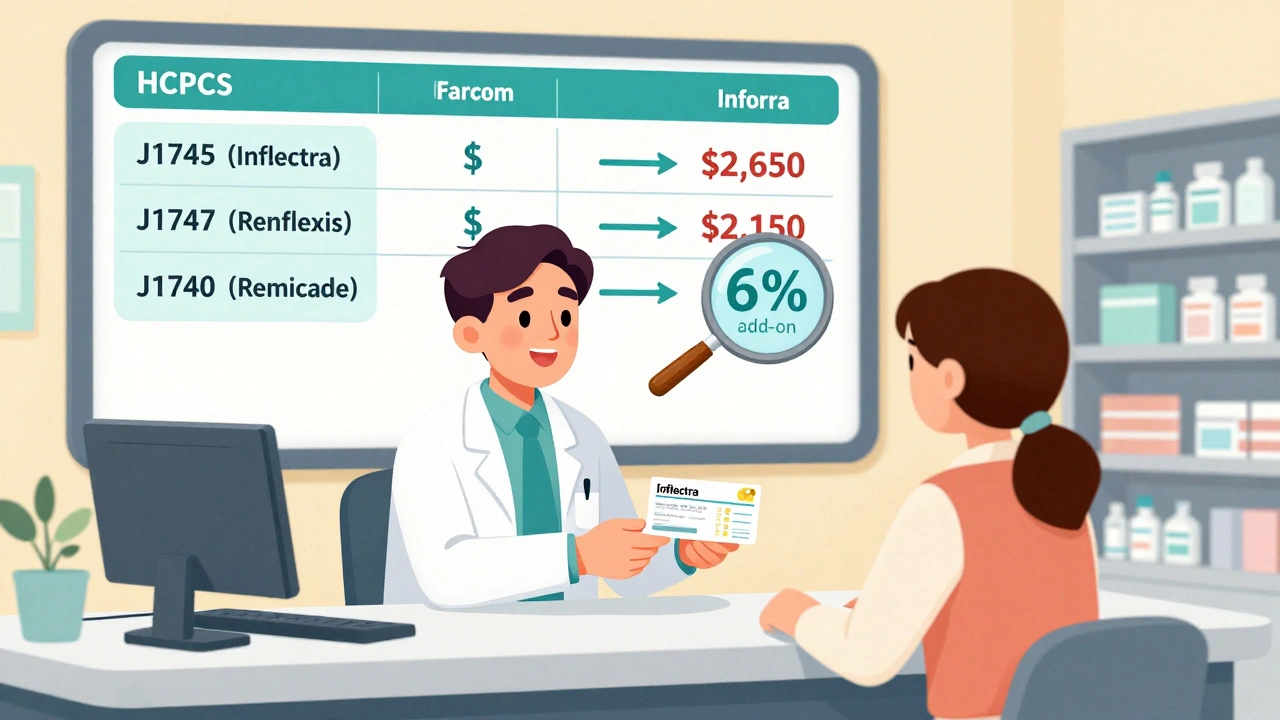
That’s why biosimilars, medications designed to match the effectiveness and safety of expensive brand-name biologics like Humira or Enbrel. Also known as biological products, they are changing how we treat autoimmune diseases, cancer, and diabetes. But they don’t just drop into the system. Each one gets its own unique HCPCS code—like J7609 for adalimumab biosimilars or J3590 for infliximab biosimilars. These codes link directly to the FDA’s list of approved biosimilars and are updated regularly. If your doctor prescribes a biosimilar, they need to use the exact code. Using the wrong one can trigger a claim rejection, even if the drug is correct.
And it’s not just about billing. HCPCS codes, standardized alphanumeric codes used across U.S. healthcare to report medical procedures, supplies, and drugs. Also known as CPT/HCPCS codes, they help track how often biosimilars are used, which ones are gaining traction, and where cost savings are happening. Insurers use this data to decide which drugs to cover and at what price. Providers rely on them to avoid audits and ensure they’re paid fairly. Patients benefit indirectly—better coding means fewer delays, fewer denials, and faster access to cheaper treatments.
You won’t find HCPCS codes for biosimilars on your pill bottle. You won’t even see them unless you’re looking at a claim form or a provider’s billing system. But they’re behind every decision that lets you get a biosimilar instead of paying thousands for the brand name. The system isn’t perfect—some providers still confuse them with generics, and some pharmacies still use old codes. But awareness is growing. And with more biosimilars hitting the market every year, getting these codes right is becoming essential.
Below, you’ll find real-world guides that show how biosimilars fit into everyday care—from how providers learn to prescribe them, to how patients can push back when insurers try to force a switch. You’ll see how coding ties into cost, safety, and access. These aren’t theoretical discussions. They’re the practical steps people are taking right now to make biosimilars work—for their health, their wallets, and their future.
Reimbursement and Coding for Biosimilars: How Billing Works Under Medicare Part B
Learn how biosimilars are billed under Medicare Part B, including HCPCS coding, reimbursement calculations, the JZ modifier, and why adoption remains low despite cost savings. Understand the system providers use and how it affects patient access.
Read more