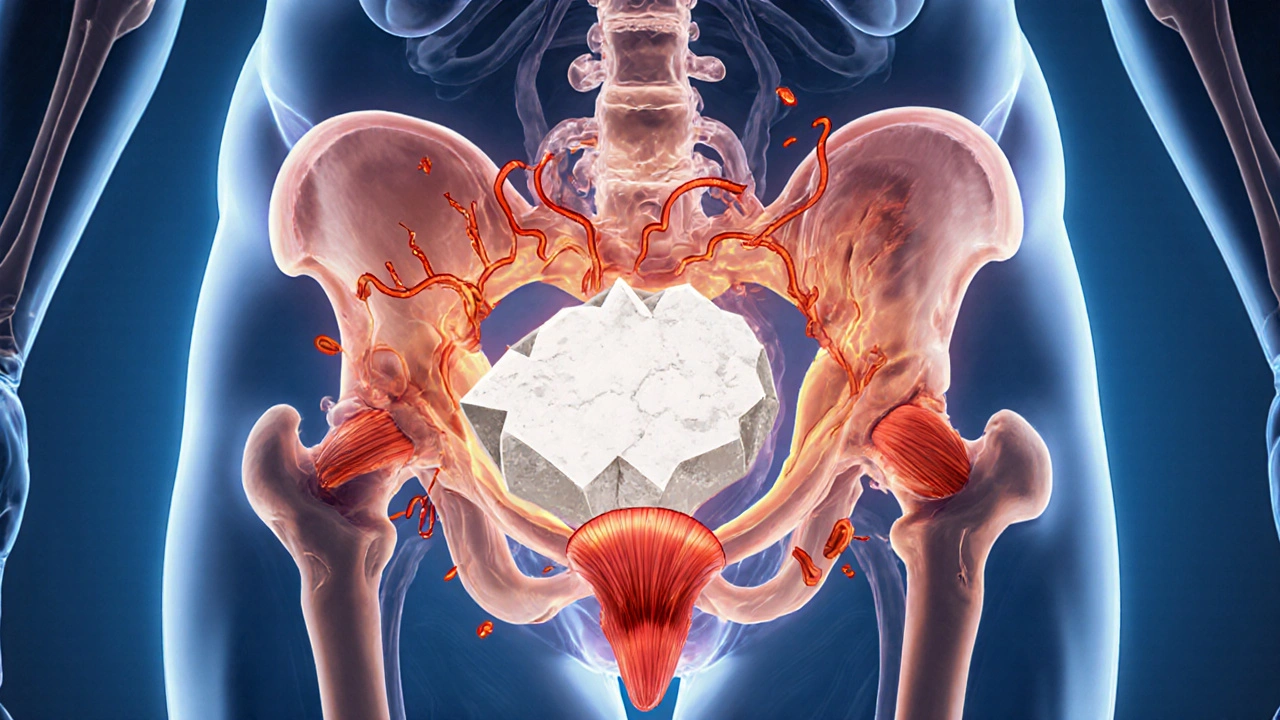
Bladder Stones: Causes, Symptoms, and Effective Treatments
When dealing with bladder stones, hard mineral deposits that develop inside the urinary bladder, often causing pain, blood in the urine, and difficulty urinating. Also known as vesical calculi, they can arise from infections, foreign bodies, or metabolic imbalances. Understanding what triggers them is the first step toward relief.
One of the biggest clues is the link between kidney stones, crystalline formations that start in the kidneys and may travel down to the bladder and bladder stones. When a kidney stone passes into the bladder, it can settle and grow, especially if the urine is concentrated or infected. This connection explains why many patients notice similar pain patterns in both the back and lower abdomen.
Infection plays a major role, too. Urinary tract infection, a bacterial invasion of the urinary system that can change urine chemistry and promote stone formation creates an environment where minerals crystallize more easily. Recurrent UTIs, especially those caused by Proteus or E. coli, raise the risk of bladder stones dramatically. Treating the infection early often prevents stones from forming or growing.
When a stone is already present, doctors evaluate several treatment paths. Lithotripsy, a non‑invasive technique that uses focused shock waves to fragment stones so they can be flushed out is a popular option for stones that are too large to pass on their own but not so hard that surgery is required. The procedure works best on stones made of calcium oxalate, the most common chemical makeup of both bladder and kidney stones, because the shock waves can shatter them into tiny pieces.
Managing and Preventing Bladder Stones
Prevention starts with lifestyle tweaks. Staying well‑hydrated dilutes the urine, making it harder for minerals to stick together. Aim for at least eight glasses of water a day, and increase intake if you live in a hot climate or exercise heavily. Reducing salt and animal‑protein intake can also lower calcium and uric acid levels, two major contributors to stone formation.
Dietary choices matter. Foods high in oxalates—spinach, beet greens, nuts, and chocolate—can increase calcium oxalate stone risk. Pairing these foods with calcium‑rich items (like dairy) can actually help bind oxalate in the gut, preventing it from reaching the kidneys and bladder. Likewise, limiting sugary drinks and excessive caffeine helps keep urine pH balanced.
Some medications influence stone risk. Loop diuretics such as Lasix (furosemide) increase calcium excretion, which may raise the chance of calcium‑based stones. On the flip side, thiazide diuretics can reduce calcium loss and are sometimes prescribed to prevent stone recurrence. Always discuss any prescription changes with your healthcare provider, especially if you’ve had stones before.
Regular monitoring is another pillar of care. If you’ve experienced a bladder stone, your doctor may order periodic ultrasounds or CT scans to catch new stones early. Simple urine tests can also flag infections or abnormal mineral levels before they become a problem.
When symptoms appear—sharp pelvic pain, blood‑tinged urine, sudden urgency, or a feeling of incomplete emptying—seek medical attention promptly. Early diagnosis often means a less invasive treatment and a quicker return to normal life.
Below you’ll find a curated selection of articles that dive deeper into related topics. From medication comparisons and side‑effect guides to lifestyle tips and the latest research on urinary health, this collection offers practical insights to help you manage and prevent bladder stones effectively.
Bladder Stones and Urinary Tract Muscle Spasms: Causes, Connection, and Relief
Explore how bladder stones trigger urinary tract muscle spasms, their shared risk factors, diagnosis, and effective treatments to prevent pain and recurrence.
Read more