Biosimilars Billing: Understanding Costs, Coverage, and Patient Access
When you hear biosimilars, complex, highly similar versions of biologic drugs approved by the FDA after the original patent expires. Also known as biologic generics, they're not the same as regular generics—they're made from living cells, not chemicals, and require far more testing to prove they work the same way. That’s why billing, the process of submitting charges to insurance for reimbursement for biosimilars is trickier than for pills. Pharmacies, hospitals, and doctors’ offices often get paid differently for biosimilars than for the brand-name versions, and insurers don’t always treat them the same way—despite lower costs.
Drug pricing, the cost structure set by manufacturers and negotiated by insurers for biosimilars can be 15% to 35% cheaper than the original biologic, but that savings doesn’t always reach patients. Some insurers still push the more expensive brand, either because of contracts or because providers aren’t trained to switch. And even when a biosimilar is chosen, insurance coverage, the extent to which a plan pays for a medication can depend on prior authorizations, step therapy rules, or confusing coding that delays payment. Patients often don’t know why their copay jumped or why their pharmacy won’t fill the cheaper version—even if their doctor prescribed it.
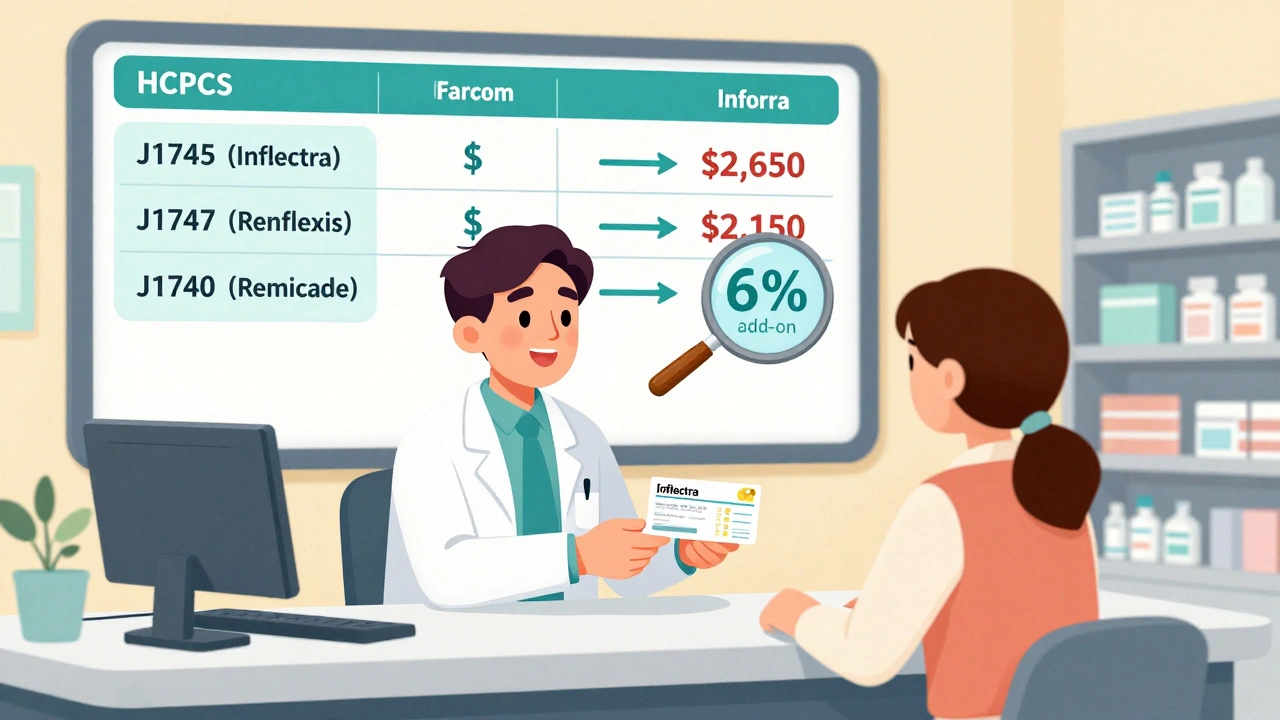
What makes this even messier is that billing for biosimilars isn’t just about the drug itself. It involves HCPCS codes, J-codes, modifier rules, and sometimes separate reimbursement tracks for infusion centers versus retail pharmacies. A single patient on a biosimilar for rheumatoid arthritis might have three different bills from three different providers—all coded differently. That’s why provider education, as covered in our posts, is critical. Many doctors still think biosimilars are riskier or less effective, not because of evidence, but because they’ve never been trained on the data.
When you look at the posts here, you’ll see why this matters. From how to talk to your doctor about staying on brand meds to how cultural beliefs shape trust in generics, everything ties back to the same problem: patients are caught in a system that doesn’t make the savings clear or easy to access. We’ve got guides on why biosimilars aren’t just cheaper versions of biologics, how education is slowly changing provider behavior, and how billing confusion leads to patients skipping doses or switching back to pricier drugs. This isn’t just about money—it’s about access, safety, and fairness in care.
Reimbursement and Coding for Biosimilars: How Billing Works Under Medicare Part B
Learn how biosimilars are billed under Medicare Part B, including HCPCS coding, reimbursement calculations, the JZ modifier, and why adoption remains low despite cost savings. Understand the system providers use and how it affects patient access.
Read more