Biosimilar Coding: What It Is and Why It Matters for Patients and Providers
When you hear biosimilar coding, a system used to identify and track biosimilar medications in healthcare records and billing. Also known as biologic coding, it’s not just paperwork—it’s what lets pharmacies, insurers, and doctors know exactly which drug you’re getting, even when it’s not the brand name. Unlike regular generics, which are simple chemical copies, biosimilars are made from living cells and are far more complex. That’s why they need special codes to avoid confusion, track side effects, and ensure you get the right treatment.
This matters because biosimilars, medications designed to be highly similar to brand-name biologics like Humira or Enbrel, but at lower cost. Also known as follow-on biologics, they’re changing how chronic diseases like rheumatoid arthritis and cancer are treated. But if the coding is wrong, your insurance might deny coverage, your pharmacy might swap your drug without telling you, or your doctor might not see your full treatment history. That’s why biologics, complex, protein-based drugs made from living organisms, often used for autoimmune and cancer conditions need clear, consistent labeling. The FDA, the U.S. agency that approves and monitors drug safety, including biosimilars and their coding standards requires unique identifiers for each biosimilar batch to trace any issues back to the source.
You might think biosimilars are just cheaper generics, but they’re not. They’re more like siblings to the original drug—not identical, but close enough to work the same way in most people. That’s why some patients and doctors are hesitant to switch. Coding helps make that switch safer by keeping a clear record of what you’ve taken. If you’ve had a bad reaction to one biosimilar, the code helps your provider know not to try another from the same family. It also lets insurers track real-world results, which affects whether they’ll cover the next round of treatment.
What you’ll find in the posts below are real stories and practical guides on how biosimilar coding affects your prescriptions, your costs, and your health. From how providers are learning to trust these drugs, to why some patients still end up on the brand name even when generics are pushed, to how culture and confusion play a role—this isn’t just about codes on a screen. It’s about your access, your safety, and your right to understand what’s in your body.
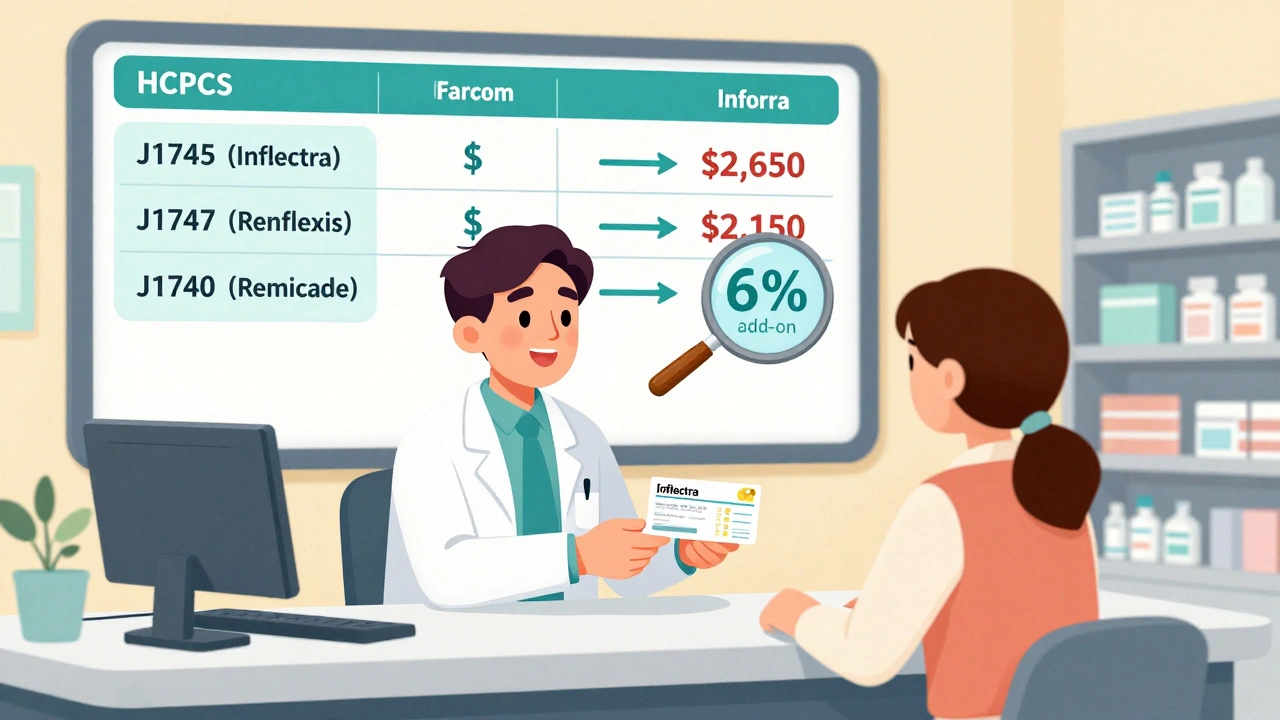
Reimbursement and Coding for Biosimilars: How Billing Works Under Medicare Part B
Learn how biosimilars are billed under Medicare Part B, including HCPCS coding, reimbursement calculations, the JZ modifier, and why adoption remains low despite cost savings. Understand the system providers use and how it affects patient access.
Read more