You’re at the park kicking the ball around with your kids, when suddenly, your breathing takes a nosedive—tight chest, wheezing, a cough that just won’t let up. Just a few decades ago, that moment could ruin your afternoon or even scare the life out of you. But today, thanks to a little inhaler filled with albuterol, you can take back control with a couple of quick puffs. If you or someone in your family deals with asthma or another lung condition, albuterol is probably as familiar in your home as keys or kettle—always within arm’s reach, just in case.
What is Albuterol and How Does It Work?
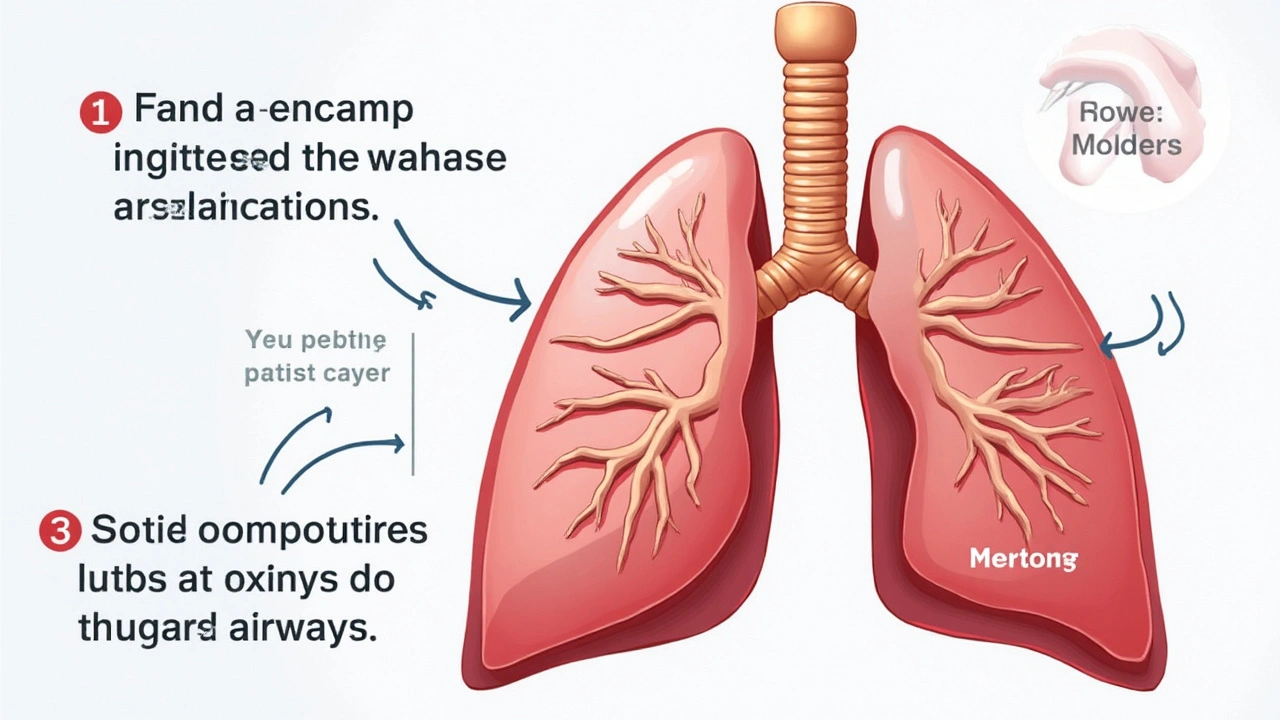
Albuterol, sometimes called salbutamol in the UK, isn’t some fancy high-tech gadget. It’s actually a type of drug known as a short-acting beta-2 agonist—try saying that after no sleep. In plain English, it’s a medicine that helps your airway muscles relax, making it easier to breathe when those airways decide to tighten up. Asthma, COPD, and a couple of other conditions basically trick your airways into thinking they need to squeeze shut. Albuterol steps in, opens things up, and lets air flow the way it should—fast.
Most people get albuterol through an inhaler, though nebulizers are used too (especially with kids or if you’re in hospital). When you breathe it in, it travels straight to those twitchy muscles in your airway and acts within minutes. That’s why it’s called a "rescue inhaler"—it works when you need it, not hours after. A quick look at the stats? The NHS estimates around 5.4 million people in the UK live with asthma, and albuterol is the most prescribed quick-relief medication for them. Simple, but life-changing.
It’s important to know that albuterol doesn’t cure asthma or stop the underlying inflammation—think of it as a fire extinguisher rather than fireproof paint. You grab it when you feel tight-chested, short of breath, or hear that familiar whistle of a wheeze. And because it acts within 5-15 minutes, it’s your fastest ticket back to normal breathing. The relief typically lasts around 4-6 hours. People often ask why they can’t just use their rescue inhaler every day to keep symptoms away, but the answer is that overusing albuterol without tackling the root of inflammation means your airways can still stay irritated, making things worse over time. Quick tip: always have a spacer (a plastic tube you attach to your inhaler) around, especially for kids—it makes it way easier to get the full dose where it needs to go.
Who Needs Albuterol?
When you hear the words "asthma inhaler," you probably picture a kid on the playground or someone puffing away during a jog, but it’s not just for children. Albuterol is prescribed for adults, teenagers, and even older folks dealing with COPD (chronic obstructive pulmonary disease), bronchitis, and sometimes exercise-induced asthma. If you have breathing issues that come and go—say, triggered by cold air, allergies, or exercise—albuterol is almost always your first line of defense.
My son, Jasper, started using an inhaler when he was barely five after a few scary trips to A&E. As a parent, nothing prepares you for that panic when your child just can’t breathe. Our GP handed us a blue inhaler loaded with albuterol and a clear action plan—what symptoms to watch for, how and when to give a dose, and how to use a spacer. Doctors tailor dosages depending on age and severity, but it’s usually one or two puffs when needed, with a max frequency set by the doctor. That said, if you need your inhaler more than three times a week, or you’re waking up at night with symptoms, your asthma probably isn’t well controlled and you might need a preventer inhaler or a dose adjustment.
Another interesting point: elite athletes sometimes need to prove they use albuterol for medical reasons, not to get a performance edge (since it slightly bumps up your heart rate and open lungs can help with endurance). The World Anti-Doping Agency does monitor usage in big sporting competitions. And, fun fact, while most people simply puff and move on, a few rare folks are actually allergic to albuterol—though it’s really uncommon. But if you notice odd hives or swelling, ring your GP just in case.
How to Use Albuterol Inhalers for the Best Results
Shaky hands and a weird taste in your mouth—that’s the classic first-time inhaler experience. But a lot of people don’t get the full benefit because they use their inhaler wrong (seriously, studies show as many as 70% of people mess up the technique). The key is timing your breath. Here’s what’s worked with Jasper and tons of others I know:
- Shake the inhaler for a few seconds before every puff. Medicine settles at the bottom and needs mixing.
- Breathe out gently. Don’t puff out too hard—just a normal, comfortable exhale to empty your lungs a bit.
- Seal your lips around the mouthpiece (or use a spacer if you have one—which is great for most people, not just kids).
- Start breathing in slowly through your mouth. The moment you start, press the inhaler down ONCE. Slow and deep is the trick here, not a quick gasp.
- Keep breathing in for about 3-5 seconds so the medicated mist actually reaches your lungs.
- Hold your breath for up to 10 seconds, if you can. This gives the medicine longer to work inside your airways.
- Breathe out gently. If your plan says two puffs, wait about 30 seconds to a minute, then repeat those steps.
If using a spacer, you don’t have to worry as much about timing because the device holds the mist for you—super handy if you’re flustered or helping a child. Just remember to rinse your mouth with water after if you use a steroid preventer inhaler, not for albuterol specifically, but it’s a good habit to have if you mix inhalers. Always check your inhaler isn’t past its expiry date, and if you hear that hissing sound but nothing comes out, you probably need a new one.
Take care of your device as well. Brits are notoriously careful with those blue inhalers, but inhalers can get clogged with dust or medicine residue, especially if tossed in a school bag or coat pocket for months. Every week, take the metal canister out, rinse the plastic bit with warm water, and let it dry completely. Never put the canister in water!
Side Effects and Safety Tips
Even though albuterol is a life-saver, it isn’t a magic cure-all. Like any medicine, you can get side effects, though most are mild. The most common? Slight tremor in your hands, jitteriness, feeling a bit wired, or a racing heartbeat. For most people, especially when they’ve had to sprint for the bus, this is no big deal—just a bit of an adrenaline rush, nothing compared to not being able to breathe. Some folks get a headache or dry mouth, but those usually pass after a few minutes.
Less common (but worth knowing): high doses of albuterol can drop your potassium, which messes with your muscles and heart rhythm. It’s rare unless you’re taking bucketloads, but always stick to the prescribed amount. If you get chest pain, a severe fast heartbeat, or feel faint after using your inhaler, go see your doctor straight away. Kids can sometimes get hyperactive or feel a bit anxious, so if you’re a parent, keep an eye out, but don’t panic—usually a good run around the garden settles things down.
Here’s a quick table showing some of the most common side effects and how likely you are to get them:
| Side Effect | Chance | Tip |
|---|---|---|
| Hand Tremor | Very Common | Usually mild, goes away quickly |
| Racing Heart | Common | Don’t use more than prescribed |
| Nervousness/Shakiness | Common | Take deep breaths, it fades |
| Headache | Less Common | Drink water, rest briefly |
| Low Potassium | Rare | If dizzy or weak, seek help |
| Allergic Reaction | Very Rare | Stop and call doctor if hives/swelling |
One more thing: overusing your blue inhaler is a red flag. If you’re needing it most days, waking at night with wheezing, or struggling with cough even after a dose, it’s a sign your asthma isn’t properly managed and you need to check in with your GP or asthma nurse for an update to your treatment plan.

Practical Advice for Families and Parents
Kids and teens are notorious for hiding stuff from their parents—albuterol inhalers included. If you’re a parent, it pays to keep tabs on whether your child’s inhaler is running out faster than usual, whether they actually know how to use it, and if their teachers or sports coaches know the plan in case of an asthma attack. Don’t assume they’ll tell you if they’re using it more—they might not want to worry you, or they just forget.
Jasper once tried to get through a football session without his inhaler during a flare-up, and we ended up at the urgent care that evening. Now he AND his coaches know: stop, take your inhaler, don’t push through. It’s worth talking with kids about signs of a flare (persistent cough, trouble talking, or chest tightness), so they know not to ignore them. For teens who sometimes skip doses, smartphone reminders or stickers (yep, the youngest ones love this) work wonders.
If you’re worried your inhaler isn’t working as well as usual, or you notice a change in symptoms, get seen sooner rather than later. Asthma UK recommends carrying a written asthma action plan—these lay out exactly when to use your inhaler, when to step up treatment, and when to get help. Store one on your phone and give copies to school or work if you need to. Remember, cold weather and viruses spike asthma attacks—you can often nip problems in the bud by using your inhaler before exposure to triggers, such as before exercise or a walk in cold wind.
There’s been an uptick in recent years, especially during spring and autumn, where pollen and pollution send kids and adults to hospital. Having a spare inhaler at school, in your car, or in a sports bag has saved many a day out. Don’t leave them in direct sunlight or somewhere super cold—the medicine can break down or freeze.
During the pandemic, some families used video calls for inhaler technique checks with their GPs. Surprisingly effective! If you’re not sure you or your child are doing it right, just ask your nurse or pharmacist—many local chemists do inhaler technique reviews on the spot.


Angie Robinson
June 14, 2025 AT 13:20Honestly, most people treat albuterol like a magic wand and ignore the real issue – chronic inflammation. You can’t just pop a couple of puffs and expect your lungs to behave. The guide glazes over the fact that over‑reliance on short‑acting beta‑2 agonists actually masks poor asthma control. If your doctor isn’t monitoring your usage, you’re basically flying blind. And yes, a spacer helps, but it’s not a cure‑all for sloppy technique. The article should have stressed the importance of a written asthma action plan much earlier. Also, the claim that albuterol is “always safe” ignores rare hypersensitivity reactions that can be serious. Bottom line: use it correctly, but don’t let it become a crutch.
Emmons Kimery
June 15, 2025 AT 17:06Totally get where you’re coming from, Angie – the rescue inhaler is a lifesaver, but it’s not a substitute for daily control meds. 👍 If you’re hitting it more than twice a week, that’s a red flag to talk to your GP. Also, using a spacer can boost delivery by up to 40%, so definitely worth the extra step. And don’t forget to check the expiration date – an old canister can lose potency fast. Keep a spare in your bag, especially if you’re active. Stay safe out there! 😊
Mimi Saki
June 16, 2025 AT 20:53Exactly, Emmons! 🌟 It’s all about balance – the inhaler gets you breathing again, but a solid preventer plan keeps the attacks at bay. If you’re ever unsure about technique, a quick pharmacist check can work wonders. Also, a little reminder: rinsing your mouth after steroid inhalers helps avoid thrush, even though albuterol alone isn’t a problem. Keep those pockets stocked and stay positive! 💪
Subramaniam Sankaranarayanan
June 18, 2025 AT 00:40Let me set the record straight for anyone still confused: albuterol is a short‑acting beta‑2 agonist designed for acute bronchospasm, not a daily maintenance drug, and using it as such betrays a fundamental misunderstanding of respiratory pharmacology. The moral imperative is to educate patients that overuse can lead to receptor desensitization, diminishing efficacy over time, which is a textbook example of iatrogenic harm. Moreover, the article's casual tone glosses over the socioeconomic disparities that affect access to spacers and proper instruction, a glaring omission in any comprehensive health discourse. It is incumbent upon clinicians to ensure that each prescription is accompanied by a demonstrable inhaler technique assessment, ideally documented in the medical record. Finally, the assertion that albuterol is universally safe neglects rare but documented cases of paradoxical bronchospasm, an adverse event that demands vigilance.
Jennifer Wees-Schkade
June 19, 2025 AT 04:26Subramaniam, you’re spot‑on about the risks of receptor down‑regulation, but let’s add some practical tips: first, always log your puffs in a diary or app – it’s easier than you think and gives your doctor solid data. Second, check the inhaler’s dose counter before each use; a low‑dose can trick you into over‑using. Third, make sure the spacer valve isn’t clogged – a quick rinse with warm water (no soap) does the trick. And finally, if you notice tremors or palpitations persisting beyond five minutes, seek medical advice immediately. These steps keep the rescue inhaler effective when you truly need it.
Kylie Holmes
June 20, 2025 AT 08:13Grab that spacer and stay on top of your inhaler game!
Fr. Chuck Bradley
June 21, 2025 AT 12:00Oh, the drama of a missed puff! Imagine standing in a soccer game, heart pounding, lungs screaming, and you’re like, “Did I even bring my inhaler?” It’s a horror story that could have been a comedy if you’d just checked your bag. The lesson? Preparation beats panic every single time.
Patrick Rauls
June 22, 2025 AT 15:46Alright folks, let’s break this down step by step. First off, albuterol is a short‑acting bronchodilator that works fast, usually within minutes, so it’s perfect for those sudden flare‑ups that catch you off guard. Second, you gotta remember to shake that inhaler – the medicine can settle at the bottom and you’ll waste a puff if you don’t mix it up properly. Third, always exhale fully before you draw in the medication; otherwise you’re just blowing air out the wrong way. Fourth, if you’ve got a spacer, use it – it helps the mist get deeper into your lungs, especially if your hands are shaky or you’re helping a kid. Fifth, after you’ve inhaled, hold your breath for about ten seconds; that gives the drug time to latch onto the airway muscles. Sixth, don’t forget to rinse your mouth if you’re also on a steroid inhaler to avoid thrush; albuterol alone doesn’t need a rinse but it’s a good habit overall. Seventh, keep an eye on the expiration date – an old canister won’t pop the same and you could end up with a dud when you need it most. Eighth, store your inhaler at room temperature, away from direct sunlight or freezing temps; extreme heat or cold can mess up the propellant. Ninth, if the inhaler makes a weird hissing sound but no spray comes out, it’s probably empty or clogged – replace it right away. Tenth, track how often you’re using it – if you’re hitting more than two or three puffs a week, that’s a signal to see your doctor about a better long‑term plan. Eleventh, if you notice side effects like jittery hands, a racing heart, or a headache that won’t quit, call your healthcare provider; it might be a dose issue. Twelfth, kids especially need supervision – a spacer and proper technique training can make a huge difference in getting the right dose. Thirteenth, teach friends or coaches the basic steps so they can help if you’re in the middle of an activity and can’t reach your inhaler quickly. Fourteenth, consider a backup inhaler in your car or at work; you never know when you’ll need it. Fifteenth, finally, stay calm – panic can worsen breathing, so take a moment to breathe slowly before you use the inhaler, and you’ll get better results. Keep these tips in mind and you’ll be ready for anything the lungs throw at you.