Imagine waking up with your skin covered in raised, itchy welts that look like giant nettle stings. They come and go, sometimes in the same spot, sometimes moving across your arms, legs, or face. You didn’t touch anything unusual. No new soap, no new food. Yet here they are - burning, throbbing, impossible to ignore. This isn’t just a rash. It’s urticaria, commonly called hives. And if you’ve had it more than six weeks, you’re not alone. About 1 in 5 people will deal with hives at some point in their life, and for many, it’s not a one-time event.
What Exactly Are Hives?
Hives aren’t caused by dirt, heat, or poor hygiene. They’re a reaction inside your body. When something triggers your immune system, mast cells in your skin release histamine - a chemical that makes blood vessels leak fluid into surrounding tissue. That’s what creates the raised, red, itchy welts you see. These patches, called wheals, can be as small as a pinhead or as big as a dinner plate. They often have a pale center and a red border. What’s strange is how fast they appear and disappear. One moment you have a hive on your arm; the next, it’s gone, and a new one pops up on your back. That’s because each individual welt lasts less than 24 hours. If they keep coming back for more than six weeks, it’s called chronic spontaneous urticaria.What Triggers Hives?
People assume hives are always from food allergies - peanuts, shellfish, eggs. But that’s only true for a small number of cases, especially in chronic hives. In fact, 70% to 80% of chronic cases have no clear trigger at all. Your body just starts reacting for no obvious reason. That’s frustrating. But when triggers do exist, they fall into a few categories:- Physical triggers: Pressure from tight clothes, cold air, heat, sweat, sunlight, or even scratching your skin can cause hives. This is called physical urticaria, and it makes up 20% to 30% of chronic cases.
- Medications: Antibiotics like penicillin, painkillers like ibuprofen or aspirin, and even some blood pressure drugs can set off reactions.
- Infections: Viral infections - especially colds or the flu - often precede outbreaks. Bacterial infections like strep throat or H. pylori (a stomach bug) are also linked.
- Autoimmune activity: In many chronic cases, your immune system mistakenly attacks your own mast cells. Around 30% to 40% of people with long-term hives have this type of internal misfire.
- Stress and hormones: Stress doesn’t cause hives directly, but it can make them worse. Hormonal changes, especially in women, also play a role - which is why women are 1.5 to 2 times more likely to get chronic hives than men.
There’s no single test to find the trigger in most chronic cases. That’s why doctors focus on managing symptoms instead of chasing a ghost cause.
Antihistamines: The First Line of Defense
If you’ve ever reached for Benadryl or Zyrtec for hives, you’ve used an antihistamine. These drugs work by blocking histamine from binding to receptors on your skin cells. No histamine binding = less swelling, less itching, fewer hives.There are two types:
- First-generation: Like diphenhydramine (Benadryl) or hydroxyzine. These work fast but make you drowsy - up to 70% of users feel sleepy. They’re fine for occasional use at night, but not for daily control.
- Second-generation: Cetirizine (Zyrtec), loratadine (Claritin), fexofenadine (Allegra). These are non-sedating for most people. They last 24 hours and are the go-to choice for daily use. The standard dose is 10mg once a day for adults.
Here’s the catch: many people don’t take enough. For chronic hives, doctors often increase the dose to 2, 3, or even 4 times the normal amount. Studies show that up-dosing helps 40% to 50% of patients who didn’t respond to regular doses. It’s not dangerous - second-generation antihistamines are safe at higher levels for long-term use.
What If Antihistamines Don’t Work?
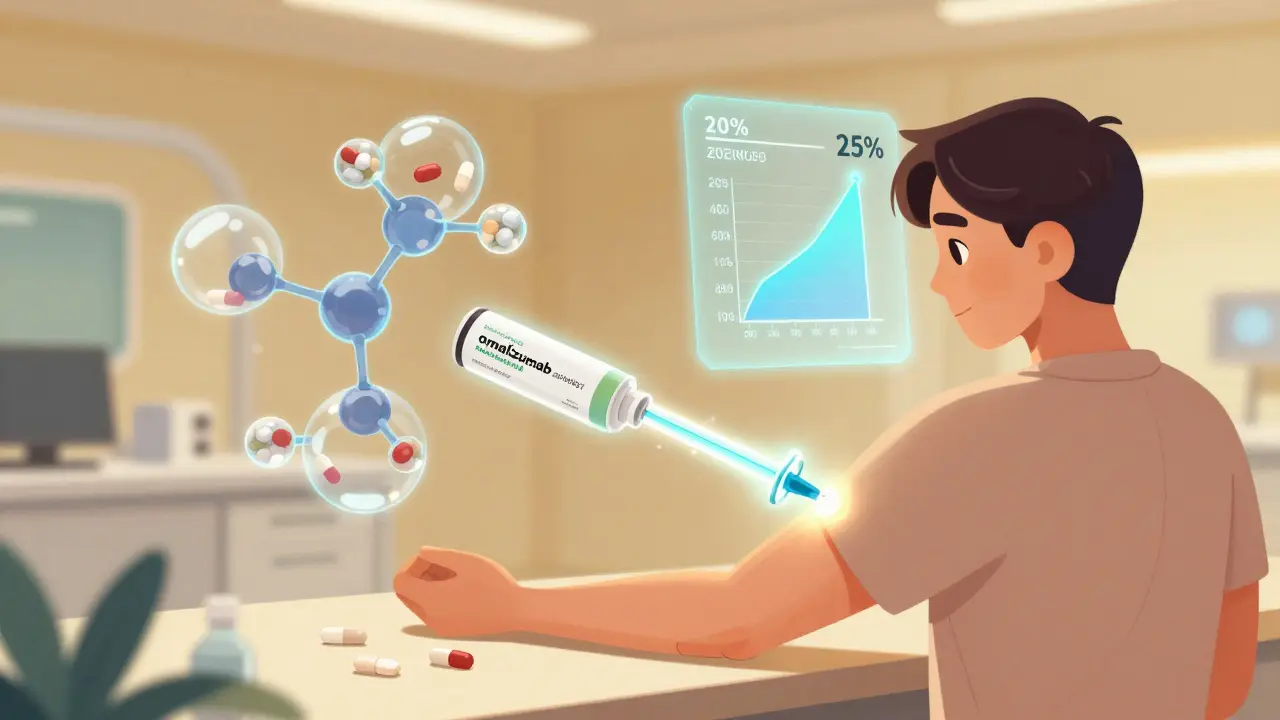
If you’ve been on the highest dose of antihistamines for 4 weeks and still breaking out, it’s time to think bigger. The next step is usually a biologic drug - a targeted therapy that stops your immune system from overreacting.One of the most common is omalizumab (Xolair). It’s an injection given every 4 weeks. In clinical trials, it helped 65% of people who didn’t respond to antihistamines. Many report complete symptom control within 4 weeks. But it’s expensive - around $1,500 per shot in the U.S. - and not everyone has access.
Then there’s dupilumab, approved by the FDA in September 2023. It’s another injectable, originally for eczema and asthma, but now also for chronic hives. In trials, 55% of patients had complete relief compared to just 15% on placebo.
The newest player is remibrutinib - a pill approved in January 2024. It’s the first oral tyrosine kinase inhibitor for hives. In trials, 45% of users had total symptom control at a dose of 50mg twice daily. The big advantage? It’s a pill. No needles. And 85% of people stick with it, compared to 70% for injections.
Corticosteroids like prednisone work fast - really fast. But they’re not for long-term use. After just 3 to 5 days, side effects kick in: high blood sugar, trouble sleeping, mood swings. One patient on NHS.uk wrote, “I felt like a different person after 3 days of prednisone.” That’s why doctors only use them as a bridge, not a solution.
Real-Life Experiences: What Patients Say
Online communities like Reddit’s r/ChronicHives have over 15,000 members. A recent survey of 1,245 people showed:- 68% said hives disrupted their sleep - many waking up 2 to 3 times a night.
- 42% stopped going to social events because they were embarrassed.
- 1 in 5 developed anxiety or depression from the constant itch and unpredictability.
Reviews of antihistamines are mixed. Cetirizine gets high marks for lasting 8 to 10 hours. But loratadine? Many say it wears off after 4 to 6 hours, forcing them to take a second dose - which isn’t recommended. Fexofenadine scores better for effectiveness but still doesn’t fully stop hives for most.
People on omalizumab report life-changing results: “I haven’t had a hive in 6 months.” But side effects like injection site pain or headaches are common. And for those without insurance, the cost is a major barrier.
How to Get Started
If you’re dealing with hives for the first time:- Start with an over-the-counter second-generation antihistamine - cetirizine 10mg once daily.
- Keep a daily log: What did you eat? Where were you? Did you sweat? Were you stressed? Did the hives appear after a shower or wearing a tight shirt?
- If they don’t improve in 2 weeks, or if they keep coming back past 6 weeks, see an allergist or dermatologist.
Don’t wait. Chronic hives aren’t dangerous in themselves, but they’re exhausting. And the longer you go without proper treatment, the harder it becomes to control them.
What to Avoid
- Don’t assume your hives are from food. Unless you’ve had a clear reaction to a specific food within minutes, it’s unlikely.
- Don’t take more than one antihistamine at a time unless your doctor says so. Combining them without guidance can increase side effects.
- Don’t use corticosteroids for more than 5 days unless you’re under close supervision.
- Don’t ignore mental health. Anxiety and depression are common side effects of chronic hives - and they make the itching worse.
The Future of Hives Treatment
The field is moving fast. Researchers are now looking at genetic markers to predict who will respond to which antihistamine. One expert predicts that within five years, blood tests could tell you whether cetirizine or fexofenadine is more likely to work for you - avoiding months of trial and error.New oral drugs like remibrutinib and linzagolix (expected FDA decision late 2024) are making treatment more convenient. And telemedicine is helping people in rural areas get specialist care without traveling hours.
But access remains unequal. In low-income countries, only 30% of chronic hives patients can get biologics. In the U.S. and Europe, it’s 85%. This gap isn’t just about money - it’s about awareness, training, and healthcare infrastructure.
The good news? Hives are manageable. You don’t have to live with constant itching. There are effective treatments. You just need to know where to look - and when to ask for help.
Are hives contagious?
No, hives are not contagious. You can’t catch them from someone else or spread them through touch. They’re caused by your own immune system reacting to internal or external triggers, not by bacteria or viruses.
Can stress cause hives?
Stress doesn’t directly cause hives, but it can trigger flare-ups or make them worse. Many people notice outbreaks during high-pressure times - exams, work deadlines, or family conflicts. Managing stress through sleep, exercise, or mindfulness can help reduce frequency.
How long do hives last?
Each individual hive lasts less than 24 hours. Acute hives go away within 6 weeks. Chronic hives last longer than 6 weeks, sometimes for months or years. The duration depends on the underlying cause - and whether treatment is adjusted properly.
Is it safe to take antihistamines every day?
Yes, second-generation antihistamines like cetirizine, loratadine, and fexofenadine are safe for daily use, even at higher doses. Studies show no serious long-term risks. First-generation antihistamines like Benadryl should not be used daily because of drowsiness and potential cognitive effects over time.
When should I see a doctor for hives?
See a doctor if hives last more than 2 weeks, if they’re interfering with sleep or daily life, if you have swelling of the lips or tongue (angioedema), or if over-the-counter antihistamines aren’t helping. Early intervention improves outcomes and prevents long-term complications.
Can diet cure hives?
There’s no proven diet that cures hives. While some people report improvement with elimination diets, studies show only a small percentage benefit - usually those with true food allergies. For chronic spontaneous urticaria, diet changes rarely make a difference. Focus on proven treatments first.
Are biologics worth the cost?
For those who haven’t responded to antihistamines, yes. Biologics like omalizumab and dupilumab can provide complete symptom control in over half of patients. While expensive, they often reduce the need for emergency visits, missed work, and other treatments. Many insurance plans cover them after standard options fail.


Jeanette Jeffrey
December 25, 2025 AT 16:46Oh wow, another ‘hives are just stress’ blog. Let me guess - you also think migraines are caused by bad vibes and psoriasis is just ‘not enough yoga’? 😒
Chronic hives aren’t a spiritual awakening, they’re an immune system glitch. And no, ‘manifesting calm’ won’t stop your mast cells from leaking histamine like a broken fire hydrant. I’ve had this for 7 years. I’ve tried acupuncture, elimination diets, crystals, and breathwork. Nothing. Only antihistamines - and even then, only at 4x the dose. Stop pretending this is a mindset issue. It’s biology, not a TED Talk.
carissa projo
December 26, 2025 AT 23:16Hey - I just want to say how much I appreciate this breakdown. Seriously. So many people treat hives like a cosmetic issue, like it’s just ‘a little itch’ - but it’s not. It’s sleepless nights. It’s canceling birthdays. It’s staring at your arms wondering if today’s the day the swelling creeps to your throat.
I started on Zyrtec, then moved to Xolair. It didn’t fix everything, but it gave me back my life. Not ‘cured’ - but managed. And that’s enough. To anyone reading this: you’re not broken. You’re not overreacting. You’re not ‘too sensitive.’ You’re just fighting a silent war inside your skin. And you’re not alone.
Keep going. Even on the days the hives win - you’re still winning just by showing up.
Jody Kennedy
December 28, 2025 AT 08:58OMG YES. I took Benadryl for years thinking it was ‘the fix’ - until I realized I was just drugged and still itchy. Switched to fexofenadine at 180mg/day and suddenly I could sleep without scratching my arms raw. Also - stress doesn’t cause it, but it’s like pouring gasoline on a fire. My flare-ups always spike before big presentations. So yeah, meditation helps… but not as much as a 3x dose of Allegra.
christian ebongue
December 29, 2025 AT 10:44antihistamines dont work for me. tried all of em. even the 4x dose. still broke out. xolair was $2k per shot. insurance denied. so i just suffer. also, the ‘dont assume it’s food’ thing? lol. i ate shrimp once. 20 mins later i looked like i got into a fight with a jellyfish. so… maybe it can be food. just not always. 🤷♂️
jesse chen
December 30, 2025 AT 10:38I just want to say… thank you for writing this. I’ve been reading forums for months, and this is the first time I’ve seen someone explain the difference between acute and chronic without sounding like a textbook. Also, the part about up-dosing? That’s huge. My doctor told me ‘take one pill’ - never mentioned 2x or 3x. I’ve been underdosing for a year. I’m going back tomorrow. Thank you. Really. You just changed my next steps.
Joanne Smith
December 30, 2025 AT 22:01Let’s be real - the ‘second-gen antihistamines are non-sedating’ line is a lie told by pharma marketers. I took Zyrtec for 8 months. I was a zombie. Numb. Dull. Couldn’t focus. My boss thought I was depressed. Turns out I was just histamine-blocked into a coma. Switched to fexofenadine - still works, but I can actually remember my own name now. Also, the ‘don’t combine antihistamines’ rule? I did it anyway. Twice. No ER visits. Just a lot of dry mouth and regret. 🤫
Alex Ragen
December 31, 2025 AT 21:37How quaint. You’ve written a 2,000-word essay on histamine receptors… while ignoring the elephant in the room: the fact that modern life is a perfect storm of environmental toxins, glyphosate-laden food, and chronic low-grade inflammation - and we’re treating it with pills that mask symptoms like a Band-Aid on a hemorrhage. The real solution? Detox. Gut healing. Low-histamine diet. But no - let’s just keep popping pills while the planet burns. Classic Western medicine. 🙄
Lori Anne Franklin
January 2, 2026 AT 21:24omg i had hives for 3 months and thought i was dying. then i started taking claritin and it was like a miracle. not 100% gone but like 90% better. i used to wear long sleeves in summer just to hide the red bumps. now i wear tank tops. i cried. not because i’m weak, but because i finally felt normal again. you’re right - you don’t have to live like this. just keep trying. even if it takes 3 meds. you got this 💪
Shreyash Gupta
January 3, 2026 AT 04:27Interesting… but you ignored the real issue: 5G radiation. 📶
My cousin in Mumbai got hives after his phone overheated. Coincidence? I think not. Also, why no mention of EMF shielding underwear? 🤔
Also, why is this so expensive in the US? In India, we just take neem leaves and pray. Works better than your fancy pills. 🙏
Ellie Stretshberry
January 4, 2026 AT 16:19i just wanted to say thank you for this. i’ve had hives for 2 years. i thought i was crazy. everyone says ‘just take an allergy pill’ like its easy. but it’s not. i cried reading the part about people skipping social events. i did that too. i felt so alone. now i feel less alone. thank you. really. 💙