Many people take statins to lower cholesterol and protect their heart. But for some, the side effects start with a dull ache in the legs, stiffness in the shoulders, or cramps that won’t go away. What seems like ordinary muscle soreness might actually be something more serious: statin-induced muscle pain. Between 10% and 30% of statin users report muscle discomfort - and not all of it is harmless. Some cases are mild and temporary. Others, like immune-mediated myositis, can lead to lasting weakness and require urgent treatment.
What’s Really Going On With Your Muscles?
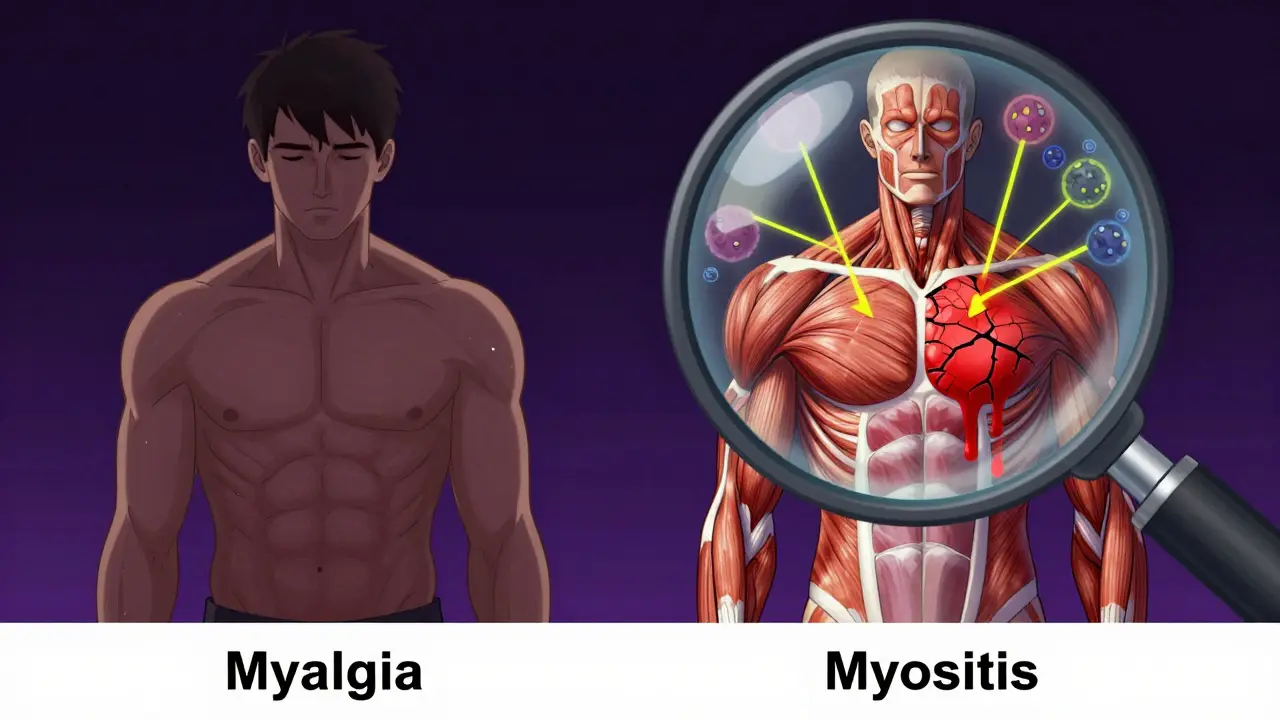
Statins work by blocking an enzyme called HMG-CoA reductase, which your liver uses to make cholesterol. But that same enzyme is also involved in producing other important compounds in your muscles - like coenzyme Q10 (CoQ10), which helps your muscle cells make energy. When statins cut CoQ10 levels by up to 40%, your muscles don’t get enough fuel. That’s one reason why you might feel tired, weak, or sore. But it’s not just about energy. Statins also mess with proteins that help regulate calcium in muscle cells. Too much calcium triggers enzymes that break down muscle tissue. Add in stress from exercise or aging, and the damage adds up. Some people develop what’s called myalgia - muscle pain without any lab markers of damage. Others develop myositis, where inflammation and muscle breakdown show up in blood tests as high levels of creatine kinase (CK), a protein that leaks out when muscles are damaged.Myalgia vs. Myositis: Know the Difference
Not all muscle pain from statins is the same. Here’s how to tell them apart:- Myalgia: Muscle aches, cramps, or stiffness without elevated CK levels. This is the most common form, affecting up to 29% of users. Symptoms usually start within weeks or months of starting a statin. Many people mistake it for normal aging or overexertion.
- Myositis: Muscle pain plus CK levels 10 to 40 times higher than normal. This means actual muscle damage is happening. You might notice trouble climbing stairs, lifting your arms, or standing up from a chair.
- Rhabdomyolysis: A rare but dangerous form where CK levels spike over 40 times normal. This can lead to kidney failure. Symptoms include dark, tea-colored urine, extreme weakness, and swelling. It’s an emergency.
- Immune-mediated necrotizing myopathy (IMNM): This is the most serious and often misdiagnosed form. It’s not just a side effect - it’s an autoimmune reaction. Your body starts attacking its own muscle tissue because it mistakes the HMG-CoA enzyme (which statins make more of) as a threat. CK levels often exceed 2,000 IU/L (normal is 30-200). Weakness gets worse over months, even after stopping the statin.
Here’s the catch: IMNM doesn’t go away when you quit statins. In fact, half of people with this condition still feel weak 6 to 12 months later. That’s why so many patients end up being misdiagnosed with fibromyalgia or chronic fatigue. One Reddit user described 18 months of worsening weakness after taking atorvastatin - it took six months of IVIG therapy before he saw improvement.
Who’s at Risk?
Some people are more likely to develop statin-related muscle problems:- Age over 50: Muscle repair slows down with age, making older adults more vulnerable.
- Being female: Women report muscle pain more often than men, though the reasons aren’t fully clear.
- Black or African descent: Studies show African Americans have 1.8 times higher risk than Caucasians, possibly due to a gene variant (SLCO1B1) that affects how statins enter liver cells.
- Taking other medications: Drugs like amiodarone, fibrates, or certain antibiotics can boost statin levels in your blood by 300-500%, increasing muscle risk.
- Low vitamin D or thyroid issues: These can worsen muscle symptoms and should always be checked.
Genetics also play a big role. The rs4149056 gene variant increases simvastatin myopathy risk from 0.6% to 1.4%. That might sound small, but for someone taking statins daily for years, it adds up.
What Doctors Should Do
If you develop muscle pain after starting a statin, your doctor shouldn’t just say, “It’s normal.” Here’s what a proper workup looks like:- Stop the statin for 2-4 weeks. If symptoms improve, that’s a strong clue.
- Test CK levels. Normal is 30-200 IU/L. Anything above 10x that needs attention.
- Check thyroid function and vitamin D. Low levels can mimic or worsen muscle pain.
- If pain persists beyond 3 months, test for anti-HMGCR antibodies. This confirms immune-mediated myopathy.
- For unclear cases, muscle MRI or electromyography (EMG) can show signs of damage - 80% of confirmed cases show myopathic changes on EMG.
Biopsy is the gold standard for diagnosing IMNM. It shows muscle fibers breaking down with almost no inflammation - a telltale sign that your immune system is attacking your muscles, not just reacting to the drug.
Treatment: What Works and What Doesn’t
For most people with mild myalgia, switching statins helps. About 73% of those who couldn’t tolerate simvastatin do fine on rosuvastatin. Others find relief with lower doses or intermittent dosing - like taking atorvastatin every other day. The IMPROVE-IT trial showed 40% of patients tolerated this approach. CoQ10 supplements (200 mg/day) sound logical - after all, statins lower CoQ10. But studies are mixed. Only 3 out of 7 trials showed real benefit. Don’t count on it as a fix. For immune-mediated myositis, you need more than supplements. Treatment requires immunosuppression:- Prednisone (1 mg/kg/day) to calm the immune system
- Methotrexate or mycophenolate to reduce long-term steroid use
- IVIG (intravenous immunoglobulin) for severe cases
- New drugs like ravulizumab (a complement inhibitor) are showing 75% response in refractory cases
Timing matters. Patients treated within 6 months of symptom onset have a 65% chance of full recovery. If treatment is delayed beyond a year, that drops to 28%.
What You Can Do Right Now
If you’re on a statin and feel off:- Don’t ignore persistent pain. Don’t assume it’s just aging.
- Track when symptoms started and how they’ve changed.
- Ask for a CK test - even if your doctor says it’s not necessary.
- Request anti-HMGCR antibody testing if symptoms last more than 3 months.
- Keep a log of all medications, including supplements and over-the-counter drugs.
- If you’re told to “just tough it out,” get a second opinion. Muscle damage can be irreversible.
Stopping statins isn’t always the end of the road. Many people switch to non-statin options like ezetimibe, PCSK9 inhibitors, or bempedoic acid - all proven to lower cholesterol without the same muscle risks. And for those who can’t tolerate any statin, newer genetic tests may soon help doctors pick the safest option before you even start.
The Bigger Picture
Statin myopathy isn’t rare - it’s underdiagnosed. The FDA logged over 21,000 cases between 2010 and 2020. Atorvastatin (Lipitor) made up 43% of those reports, even though it’s not the most prescribed statin. That tells us something: not all statins are equal. Some are more likely to cause trouble. And here’s the hard truth: stopping statins because of muscle pain increases your risk of heart attack or stroke by 25% over 10 years - especially if you’re high risk. That’s why finding a solution matters. It’s not about choosing between heart health and muscle comfort. It’s about finding the right balance - the right drug, the right dose, the right timing.Future tools - like polygenic risk scores that predict who’s likely to have side effects - could change everything. By 2030, doctors may use your DNA to pick your statin before you even take your first pill. Until then, awareness, testing, and persistence are your best tools.
Can statin muscle pain go away on its own?
Yes - but only if it’s simple myalgia. Most people with mild muscle aches and no elevated CK levels see improvement within 1-2 weeks after stopping the statin. However, if you have myositis or immune-mediated necrotizing myopathy, symptoms often get worse after stopping the drug and won’t resolve without treatment. Don’t assume all muscle pain will disappear on its own.
Is CoQ10 supplementation effective for statin muscle pain?
The evidence is weak. While statins lower CoQ10 levels, only 3 out of 7 clinical trials showed meaningful improvement in muscle symptoms with CoQ10 supplements. Most major guidelines don’t recommend it as a standard treatment. It’s unlikely to help if you have true muscle damage or autoimmune myositis.
Can I switch to a different statin if I have muscle pain?
Yes, many people can. About 73% of those who couldn’t tolerate simvastatin tolerate rosuvastatin. Pravastatin and fluvastatin are also less likely to cause muscle issues because they’re processed differently by the liver. But if you’ve had myositis or high CK levels, switching isn’t guaranteed to work - and you need monitoring. Immune-mediated myopathy often doesn’t improve with any statin.
How do I know if I have immune-mediated myositis?
Look for these signs: muscle weakness that keeps getting worse after stopping the statin, CK levels above 2,000 IU/L, symmetric weakness in hips and shoulders, and no improvement after 3 months. Blood tests for anti-HMGCR antibodies are the key diagnostic tool. If positive, you need a neuromuscular specialist - not just a general practitioner.
What happens if I ignore statin muscle pain?
Mild myalgia might just be annoying. But ignoring true myositis or immune-mediated myopathy can lead to permanent muscle damage, loss of mobility, and long-term disability. In rare cases, rhabdomyolysis can cause kidney failure. Delayed diagnosis of immune-mediated myopathy cuts your chance of full recovery by more than half. Early action saves muscle and function.
Next Steps: What to Ask Your Doctor
If you’re experiencing muscle pain while on a statin, here’s what to say next time you see your doctor:- “I started feeling this pain after beginning [name of statin]. Can we check my CK levels?”
- “Could this be immune-mediated myopathy? Can I get tested for anti-HMGCR antibodies?”
- “Are there non-statin options that work just as well for my heart?”
- “Could any of my other medications be making this worse?”
- “If I stop this statin, what’s the plan to protect my heart?”
Statin-induced muscle pain isn’t a one-size-fits-all problem. For some, it’s a minor inconvenience. For others, it’s a signal of a deeper immune problem. The key is not to ignore it - and not to accept “it’s normal” as an answer. Your muscles matter. Your heart matters. You deserve both to be protected.

Brian Anaz
January 6, 2026 AT 02:50Venkataramanan Viswanathan
January 7, 2026 AT 13:41Vinayak Naik
January 7, 2026 AT 14:25Lily Lilyy
January 8, 2026 AT 22:01Susan Arlene
January 10, 2026 AT 20:02Joann Absi
January 12, 2026 AT 03:23Ryan Barr
January 12, 2026 AT 11:45Dana Termini
January 13, 2026 AT 00:45Mukesh Pareek
January 14, 2026 AT 06:49Ashley S
January 15, 2026 AT 06:35Jeane Hendrix
January 17, 2026 AT 05:55