Akathisia vs. Restless Legs Syndrome Checker
This tool helps you distinguish between akathisia and restless legs syndrome based on your symptoms and medication history. Both conditions involve restlessness but require different treatments.
Answer these questions to get your results
Please answer these questions honestly for the most accurate results.
Imagine taking a medication to help with anxiety or psychosis, only to feel like you’re being pulled apart from the inside. Your legs won’t stop moving. You can’t sit still. You feel like you need to pace, shift, or jump out of your skin - but you’re not anxious. You’re not hyper. You’re just unbearably restless. This isn’t just stress. It could be akathisia - a hidden, often misdiagnosed side effect of common psychiatric drugs. And it’s not the same as restless legs syndrome, even though they feel alike.
What Is Akathisia, Really?
Akathisia isn’t just fidgeting. It’s a neurological reaction triggered by certain medications, especially antipsychotics like haloperidol, risperidone, and even some antidepressants or anti-nausea drugs like metoclopramide. First described in the 1950s, it’s now one of the most common side effects of these drugs - affecting 20-40% of people on older antipsychotics and 5-15% on newer ones. The key sign? An intense, internal urge to move. It’s not about being nervous or impatient. It’s a physical torment. People describe it as:- Aching restlessness that makes you feel like your bones are vibrating
- Needing to pace, cross and uncross your legs, rock back and forth, or shift weight constantly
- Feeling like you can’t sit still even for a minute - even when you’re exhausted
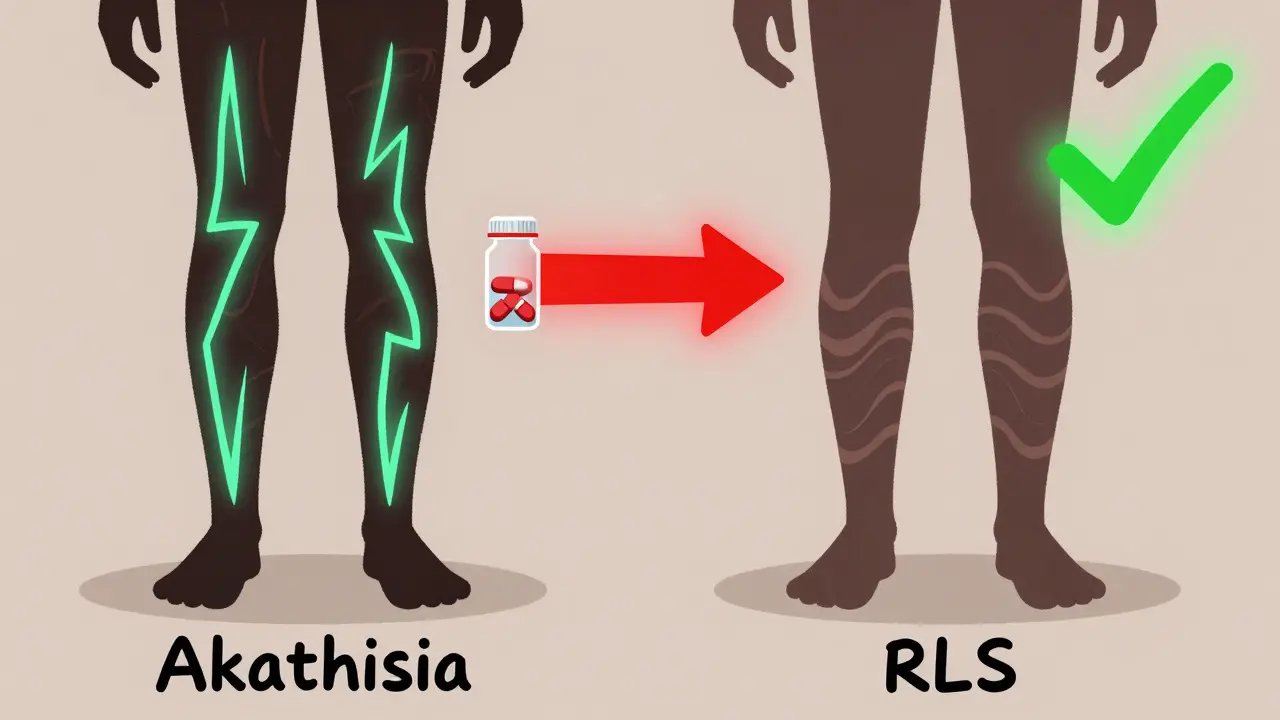
How Is It Different from Restless Legs Syndrome?
Restless legs syndrome (RLS) and akathisia both involve leg discomfort and movement, but they’re not the same. Confusing them can lead to the wrong treatment - and real harm.| Feature | Akathisia | Restless Legs Syndrome (RLS) |
|---|---|---|
| When it happens | While sitting or standing, anytime of day | Mainly at night or during rest |
| Where you feel it | Whole body - inner tension, not just legs | Primarily legs, sometimes arms |
| What relieves it | Moving helps, but doesn’t fully fix the inner distress | Moving gives clear, lasting relief |
| Trigger | Starts after taking certain meds (antipsychotics, metoclopramide) | Often genetic, linked to iron deficiency or kidney disease |
| Response to dopamine meds | Worsens with levodopa or pramipexole | Improves with levodopa or pramipexole |
| Treatment | Reduce or stop the drug; propranolol, clonazepam | Iron supplements, gabapentin, dopamine agonists |
Why Misdiagnosis Is Dangerous
In 2017, a case study in the Royal Australian College of General Practitioners journal showed a patient on haloperidol developing severe akathisia. The doctor thought it was worsening psychosis. The dose was doubled. Within days, the patient had suicidal thoughts. That’s not rare. Studies show up to half of akathisia cases are misdiagnosed. And the consequences are serious:- Increased risk of suicide - akathisia is linked to suicidal ideation more than the underlying illness
- Aggression and violence - patients describe feeling out of control
- Medication non-adherence - people stop taking their meds because the side effects feel worse than the illness
How Doctors Diagnose It
There’s no blood test or scan for akathisia. Diagnosis is clinical - meaning it’s based on what the patient says and what the doctor sees. The gold standard is the Barnes Akathisia Rating Scale (BARS). It takes 5-10 minutes and asks two things:- Subjective: “Do you feel an inner restlessness that makes you feel like you must move?”
- Objective: “Can you see the patient pacing, rocking, or shifting legs repeatedly?”
- Check when symptoms started - right after a new drug or dose change?
- Rule out other movement disorders like Parkinson’s or tardive dyskinesia
- Ask if movement helps - in RLS, movement brings relief; in akathisia, it only eases the tension briefly
What to Do If You Think You Have It
If you’re on an antipsychotic, metoclopramide, or similar drug and feel this kind of restlessness:- Don’t stop the medication cold. Sudden withdrawal can make things worse or trigger other problems.
- Write down your symptoms. When did they start? What exactly do you feel? How often do you move? Keep a log.
- Ask your doctor: “Could this be akathisia?” Show them the Barnes scale if needed.
- Request a medication review. Is there a lower-dose option? A different drug with less akathisia risk?
Treatment Options
The first step is always reducing or stopping the drug causing it - if possible. For haloperidol, tapering over 3 days has been shown to resolve symptoms safely. If you can’t stop the medication (because your psychosis is severe), doctors can add treatments:- Propranolol (10-60 mg daily): A beta-blocker that calms the nervous system. Often the first choice.
- Clonazepam (0.5-2 mg nightly): A benzodiazepine that reduces inner tension. Effective but risk of dependence.
- Cyproheptadine (4 mg daily): An antihistamine that blocks serotonin. Used off-label with good results.
What Patients Are Saying
On Reddit’s r/antipsychotics, users share stories like:“My doctor said I was just anxious. He doubled my Seroquel. I couldn’t sleep. I paced all night. I thought I was going crazy. Then I read about akathisia on Wikipedia. I begged to stop the drug. Three days later, I felt human again.” - RestlessMind2023A 2022 survey by NAMI found 68% of people with medication-induced restlessness were misdiagnosed with anxiety. 42% had their dose increased - and got worse. One former patient wrote: “Akathisia was the most torturous thing I’ve ever experienced. Worse than the psychosis.”
What You Can Do Now
If you’re taking antipsychotics or metoclopramide:- Know the signs: inner restlessness + need to move = possible akathisia
- Track your symptoms: use a simple journal
- Ask your doctor to use the Barnes scale
- Bring this article with you
The Bottom Line
Akathisia isn’t rare. It’s hidden. And it’s deadly if missed. It’s not anxiety. It’s not laziness. It’s a neurological side effect - and it’s treatable. The real problem isn’t the medication. It’s the lack of awareness. Clinicians need to ask the right questions. Patients need to speak up. And if you’re feeling this kind of restlessness - don’t wait. Don’t assume it’s just stress. Ask: “Could this be akathisia?” Because sometimes, the thing meant to save you is the thing making you suffer - and you don’t have to live with it.Can akathisia go away on its own?
Yes, but only if the triggering medication is reduced or stopped. Akathisia doesn’t resolve on its own while you’re still taking the drug. In many cases, symptoms improve within days of lowering the dose. For example, one case study showed complete relief within 3 days of stopping haloperidol. If the drug is continued, akathisia can become chronic or even permanent in rare cases.
Which medications are most likely to cause akathisia?
First-generation antipsychotics like haloperidol and fluphenazine carry the highest risk due to strong dopamine-blocking effects. Second-generation drugs like risperidone and olanzapine also cause it, but less often. Non-psychiatric drugs like metoclopramide (for nausea) and certain antidepressants (especially SSRIs like fluoxetine) can also trigger it. The risk increases with higher doses and rapid dose changes.
Is akathisia the same as anxiety?
No. Anxiety is a mental state - worry, fear, racing thoughts. Akathisia is a physical movement disorder caused by brain chemistry changes from medication. People with akathisia often feel calm mentally but are physically unable to sit still. The inner tension feels like a physical ache, not emotional fear. Many patients describe it as being trapped in their own body. Mistaking it for anxiety leads to dangerous treatment errors.
Can I still take my antipsychotic if I have akathisia?
It depends. For mild cases, adding propranolol or clonazepam may allow you to continue the antipsychotic. For severe cases, switching to a lower-risk drug like lumateperone or reducing the dose is safer. Never stop abruptly. Work with your doctor to find a balance between controlling your mental health condition and managing side effects. The goal isn’t always to stop the drug - it’s to stop the suffering.
Are there any new treatments for akathisia?
Yes. Pimavanserin (Nuplazid), originally for Parkinson’s hallucinations, reduced akathisia by 62% in a 2023 trial. Transcranial magnetic stimulation (TMS) is being tested at Harvard as a non-drug option. Also, new antipsychotics like lumateperone are designed with lower akathisia risk. An AI-powered app launched in 2023 by the Movement Disorder Society helps clinicians spot movement patterns during telehealth visits - improving early detection.
How long does akathisia last after stopping the drug?
In acute cases, symptoms usually fade within days to weeks after stopping the medication. Chronic akathisia lasts longer than 6 months and may persist even after stopping the drug, especially if it went untreated for a long time. Tardive akathisia can appear months after stopping, which is why long-term monitoring matters. Withdrawal akathisia can occur within 6 weeks of dose reduction and often resolves with re-introduction or supportive treatment.


Lance Nickie
January 14, 2026 AT 08:20Clay .Haeber
January 15, 2026 AT 16:51Nelly Oruko
January 16, 2026 AT 08:12Angel Tiestos lopez
January 18, 2026 AT 04:56Scottie Baker
January 18, 2026 AT 19:40Anny Kaettano
January 20, 2026 AT 13:39Kimberly Mitchell
January 22, 2026 AT 08:42Diana Campos Ortiz
January 23, 2026 AT 03:42Jesse Ibarra
January 24, 2026 AT 17:38laura Drever
January 26, 2026 AT 10:55Rosalee Vanness
January 26, 2026 AT 15:24Lethabo Phalafala
January 28, 2026 AT 00:34Milla Masliy
January 28, 2026 AT 21:45Damario Brown
January 29, 2026 AT 09:55sam abas
January 30, 2026 AT 01:01