OTC Medication Safety Checker
Check Your Medication Safety
Identify potential risks when using over-the-counter medications with your health conditions.
Your medication safety check will appear here
When a medicine moves from prescription-only to over-the-counter (OTC), it seems like a win: easier access, lower cost, no doctor’s visit needed. But that shift isn’t just paperwork-it changes how you use the drug, and not always for the better. Many people think OTC means "safe for anyone," but that’s a dangerous assumption. The truth is, OTC switches come with hidden risks you won’t find on the label.
Why Do Medications Switch from Prescription to OTC?
The FDA doesn’t let drugs jump from prescription to OTC lightly. It takes years of data showing the medicine is safe for self-use. The goal? Make common treatments easier to get while cutting down on doctor visits. For example, ibuprofen was prescription-only until 1984. After proving it was safe for short-term pain and fever, it became a shelf staple. Today, you can buy it for $5 instead of $40 a month. That’s a big win for wallets. But here’s what most people don’t realize: when a drug becomes OTC, it doesn’t just get cheaper-it gets used by more people, often without knowing why or how. A 2009 study found that as OTC use expands, so does the chance of misuse. No doctor is there to check your history, your other meds, or your health conditions. That’s where problems start.The Hidden Dangers of Self-Medication
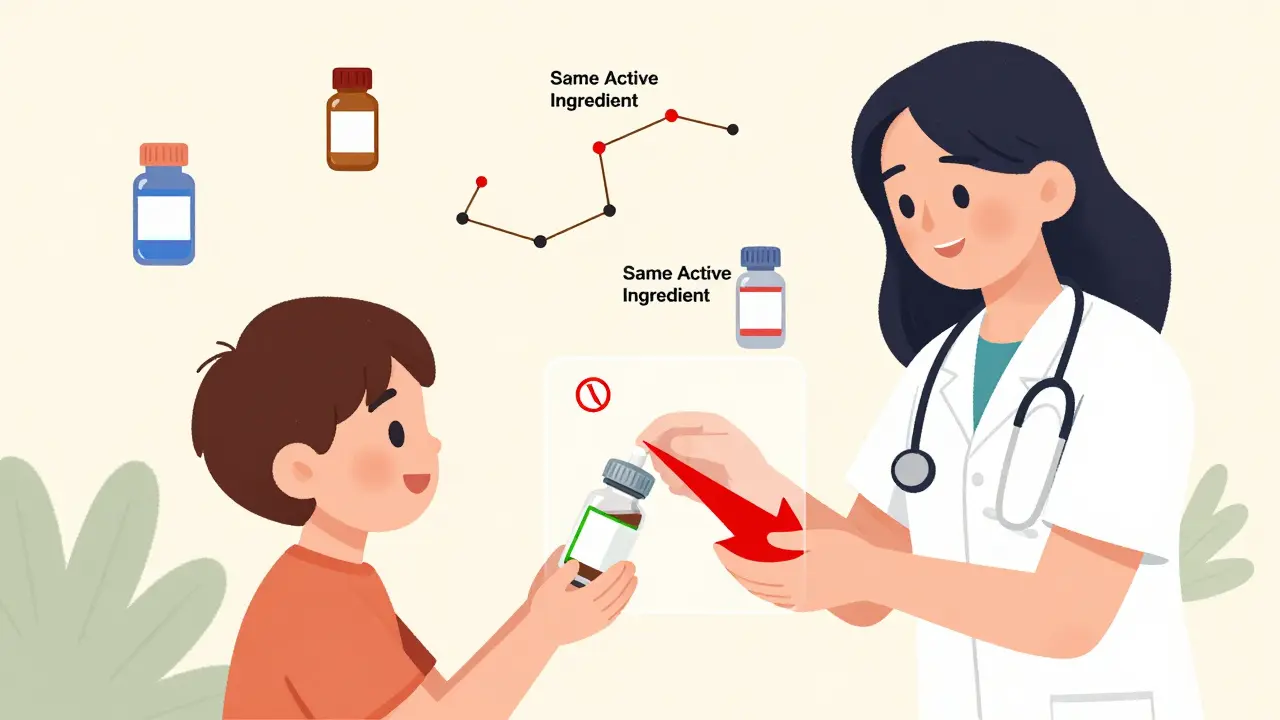
OTC drugs aren’t harmless snacks. They’re still powerful chemicals. Take acetaminophen-the active ingredient in Tylenol. It’s fine at the right dose. But take two different cold medicines, both with acetaminophen, and you can easily hit the toxic limit. That’s how liver damage happens. One Reddit user, PharmTech2020, shared how they’ve seen patients double up on OTC painkillers because they didn’t realize both products had the same active ingredient. It’s more common than you think. NSAIDs like ibuprofen and naproxen are another big risk. Used long-term, they can cause stomach ulcers, kidney failure, or even heart attacks. People with high blood pressure, diabetes, or kidney disease are especially vulnerable. Yet, most OTC labels don’t scream "DANGER"-they just list a few warnings in tiny print. And if you’re over 65? The American Geriatrics Society says 30 OTC drugs are risky for you, including diphenhydramine (Benadryl), which can cause confusion and falls. Then there’s pseudoephedrine, the decongestant in cold medicines. It’s fine for most people. But if you’re on an antidepressant like an MAOI, mixing them can spike your blood pressure to dangerous levels. A 2023 study from Ohio State University called this combination "potentially life-threatening." And yet, you can still buy it off the shelf-just behind the counter, with ID. That’s not safety. That’s a half-measure.Who’s Most at Risk?
Not everyone handles OTC drugs the same way. Certain groups are far more likely to get hurt:- Older adults: Their bodies process drugs slower. Many take five or more medications daily. A simple OTC sleep aid can clash with blood pressure pills, causing dizziness or fainting.
- People with chronic conditions: Diabetes, heart disease, liver or kidney problems? OTC meds can make things worse. NSAIDs can harm kidneys. Antihistamines can raise blood sugar.
- Those on multiple prescriptions: If you’re on three or more meds, the chance of a bad interaction jumps. OTC drugs don’t get checked in electronic health records. Your pharmacist might not know what you’re taking unless you tell them.
- Parents and caregivers: Kids’ dosing is tricky. Giving too much acetaminophen or ibuprofen by accident is a top reason for ER visits.
What the Label Doesn’t Tell You
All OTC drugs must follow the FDA’s "Drug Facts" label format. It looks simple: active ingredients, uses, warnings, directions. But here’s the catch: most people don’t read it. A 2022 survey found only 32% of users consistently read the full label. And even if they do, the wording can be vague. For example, a label might say: "Do not use if you have high blood pressure." But what does that mean? Is it safe if your pressure is 135/85? What if you’re on a beta-blocker? The label doesn’t explain. That’s why you need to go beyond the box.How to Use OTC Medicines Safely
You don’t need to avoid OTC drugs. You just need to use them smarter. Here’s a simple three-step rule:- Check the warnings. Look for phrases like "Do not use if you have..." or "Ask a doctor before use if you have..." If you have any chronic condition, take that seriously.
- Compare active ingredients. Never take two OTC meds with the same active ingredient. Check every pill, syrup, or patch. Acetaminophen, ibuprofen, diphenhydramine, and pseudoephedrine are the most common culprits for accidental overdose.
- Ask your pharmacist. Pharmacists are trained to spot interactions. Tell them what you’re taking-prescription, OTC, vitamins, even herbal supplements. They’re not just cashiers. They’re your last line of defense.
What’s Changing? New Tools for Safer Use
The FDA is trying to fix the problem. In 2022, they updated the Drug Facts label to use bigger fonts, clearer language, and better organization. They’re also pushing for real-world data tracking-using apps and EHRs to catch adverse events after a drug hits the shelf. Some pharmacies are testing QR codes on packaging. Scan it, and you get a video explaining the risks, interactions, and what to watch for. Walmart started this pilot in 2023 with 15% of their private-label OTC products. It’s early, but it’s a step in the right direction. Still, technology won’t fix human behavior. The biggest risk isn’t the drug-it’s the belief that OTC means "no risk." As Dr. David Kaelber from Case Western says, "People don’t realize they’re taking a medication." That mindset is the real problem.When to Call Your Doctor
OTC meds are great for short-term relief: a headache, a stuffy nose, heartburn. But if symptoms last more than a few days-or get worse-you need a doctor. Self-diagnosing can delay real treatment. A persistent cough might be allergies. Or it might be early heart failure. A fever that won’t break could be a simple virus-or something like Lyme disease. Dr. Michael Ruffin puts it simply: "Tell your family doctor when the symptom started." That’s the key. OTC drugs mask symptoms. They don’t fix causes. And masking too long can be deadly.Final Thought: OTC Isn’t Risk-Free
The move from prescription to OTC isn’t about convenience. It’s about trust-trust that you’ll read the label, trust that you’ll check for interactions, trust that you’ll know when to stop and call a professional. Most people can handle it. But not all. If you’re taking multiple meds, have chronic health issues, or are over 65, treat every OTC pill like a prescription. Ask questions. Read the label twice. Talk to your pharmacist. Your body doesn’t care if the drug is "over-the-counter." It only cares if you’re using it safely.Are OTC drugs really safe if they don’t need a prescription?
OTC drugs are safe when used exactly as directed-but only if you understand your own health. Many people assume "no prescription" means "no risk," but that’s not true. OTC drugs can cause serious side effects, especially when mixed with other medications or taken by people with conditions like high blood pressure, kidney disease, or liver problems. Always read the label and talk to a pharmacist if you’re unsure.
Can I take OTC painkillers every day for chronic pain?
No. Long-term use of NSAIDs like ibuprofen or naproxen can lead to stomach ulcers, kidney damage, or heart problems-even if you feel fine. If you’re using OTC pain meds daily for more than 10 days, you need to see a doctor. Chronic pain isn’t something to manage with shelf-stable pills. There are safer, more effective treatments available with medical supervision.
How do I know if two OTC medicines have the same active ingredient?
Look at the "Active Ingredients" section on the Drug Facts label. Common ones include acetaminophen (Tylenol), ibuprofen (Advil), diphenhydramine (Benadryl), and pseudoephedrine (Sudafed). Many cold, flu, and sleep aids contain the same ingredients. If you’re taking more than one product, compare the labels side by side. If the active ingredient matches, don’t take them together.
Why are older adults more at risk with OTC meds?
As we age, our bodies process drugs more slowly, and we often take multiple medications. This increases the chance of dangerous interactions. OTC drugs like diphenhydramine (found in sleep aids) can cause confusion and falls in seniors. NSAIDs raise the risk of stomach bleeding by 2 to 4 times. The American Geriatrics Society lists 30 OTC drugs as potentially unsafe for people over 65. Always check the Beers Criteria before taking anything new.
Should I tell my doctor about OTC meds I’m taking?
Yes. Always. Many doctors don’t ask about OTC drugs because they assume they’re harmless. But they’re not. OTC meds can interfere with prescriptions, worsen chronic conditions, or mask symptoms that need attention. Make a list of everything you take-prescription, OTC, vitamins, herbs-and bring it to every appointment. It could save your life.


Aliza Efraimov
December 30, 2025 AT 11:11I used to think OTC meant "safe," until my mom ended up in the ER from mixing Tylenol and a cold med. She didn’t even know they had the same active ingredient. I swear, if there was a warning siren when you scanned a barcode, we’d save so many lives. Pharmacies need to do more than just shove these on shelves and hope for the best.
It’s not just about reading labels-most people don’t have the time, energy, or literacy to parse that tiny print. We need better design, not just better warnings.
Nisha Marwaha
December 30, 2025 AT 16:07From a pharmacovigilance standpoint, the OTC switch paradigm operates under the assumption of pharmacokinetically homogenous populations, which is fundamentally flawed. The absence of prescriber-mediated risk stratification introduces significant pharmacodynamic heterogeneity, particularly in polypharmacy cohorts. The Beers Criteria remain underutilized in consumer-facing contexts, and regulatory frameworks lag behind real-world usage patterns.
What’s needed is a tiered OTC classification system-Class I (low risk), Class II (conditional), Class III (restricted)-with mandatory digital labeling via QR codes linked to dynamic interaction alerts. Until then, we’re just gambling with public health.
Russell Thomas
January 1, 2026 AT 12:30Oh wow, a whole article about how people are dumb for not reading labels? Groundbreaking. I’m sure the FDA is just sitting around crying because nobody bothered to open the box. Maybe if they made the warnings bigger than the product name, people would notice.
Meanwhile, my grandma takes Benadryl every night because it "helps her sleep," and she’s got a heart condition. But hey, it’s OTC, so who cares? Let her keep doing it until she forgets her own name. That’s freedom, baby.
Nicole K.
January 3, 2026 AT 10:08If you’re too lazy to read a label, you deserve to get hurt. This isn’t rocket science. Don’t mix stuff. Don’t take it if you’re old or sick. Simple. No one forced you to take it. If you can’t handle basic responsibility, maybe you shouldn’t be allowed to buy medicine at all.
Stop treating adults like children. The problem isn’t the drug-it’s the people who think they’re entitled to be safe without trying.
Fabian Riewe
January 4, 2026 AT 14:56Big respect to the author for calling this out. I’m a pharmacy tech and I see this every day. People grab three different cold meds, think they’re "stacking" for extra power, and then wonder why they’re dizzy or nauseous.
My favorite thing to do? Ask, "What else are you taking?" and watch their face when they realize they’ve been taking acetaminophen in three different forms. Half the time, they didn’t even know.
Just remember: OTC doesn’t mean "no consequences." It means "you’re on your own now." Be smart.
Amy Cannon
January 4, 2026 AT 22:43As someone who has spent considerable time in both the United States and India, I have observed that the cultural perception of over-the-counter pharmaceuticals is starkly divergent. In the U.S., there is an almost religious faith in the infallibility of the FDA and the clarity of the Drug Facts label, whereas in India, OTC medications are often acquired from street vendors with no labeling whatsoever.
Yet, despite the disparity in access, the underlying issue remains identical: a profound lack of pharmaceutical literacy. The solution, therefore, cannot be purely regulatory. It must be educational. We must integrate basic pharmacology into high school curricula. We must teach people how to read a label like they read a menu. Because if you don’t know what’s in it, you shouldn’t put it in your body.
Jim Rice
January 6, 2026 AT 07:22Stop pretending this is a public health crisis. People have been taking aspirin since the 1800s without a doctor. If you can’t figure out not to take two things with acetaminophen, maybe you shouldn’t be allowed to use a smartphone.
The real problem? Lawyers. Insurance companies. The FDA’s fear of lawsuits. They turned a simple, safe practice into a panic-inducing lecture. You want safety? Don’t give people information. Give them a pill with no label. Then they’ll have to ask someone. Maybe that’s the real solution.
Henriette Barrows
January 7, 2026 AT 09:04I’m so glad this got written. I used to be the person who took Advil every day for back pain and thought it was fine because it was "just OTC." Then I started getting stomach cramps. My doctor said I’d almost given myself an ulcer.
It’s not about being scared-it’s about being aware. I wish someone had told me earlier. Now I always check the label, ask my pharmacist, and if it’s been more than 10 days? I call my doctor. It’s not a big deal. It’s just smart.
Alex Ronald
January 9, 2026 AT 09:03One thing that’s rarely discussed: OTC switches reduce access for people who can’t afford prescriptions, but they also remove the gatekeeping that ensures people get screened for contraindications. The trade-off is real.
I work with low-income patients. Many of them use OTC meds as their only access to pain relief. But they also have diabetes, hypertension, or kidney disease. They don’t know the risks. They’re not dumb-they’re underserved.
We need community health workers trained to walk people through labels-not just more warnings.
Teresa Rodriguez leon
January 9, 2026 AT 21:32My ex took 8 Tylenol a day for his headaches. Said he "didn’t want to bother the doctor." He ended up with liver failure. He’s fine now, but he had to get a transplant. He didn’t even know the label said "do not exceed 4,000 mg." He thought "extra strength" meant "take more."
It’s not just about reading. It’s about understanding. And most people don’t.
Manan Pandya
January 11, 2026 AT 06:43As someone who grew up in a household where OTC medicines were treated like candy, I can confirm: education is the missing link. My mother used to give me children’s ibuprofen for my migraines because "it’s safer." She didn’t know the dose was for kids.
What’s needed isn’t more regulation-it’s more outreach. Community pharmacies should offer 5-minute label-reading workshops. Schools should include basic pharmacology in health classes. This isn’t a failure of the public-it’s a failure of systems to meet people where they are.
Paige Shipe
January 13, 2026 AT 01:32People are idiots. They don’t read labels. They don’t care. They just want quick fixes. And now we have a whole generation of people who think a pill is a solution, not a tool. You want to fix this? Ban OTC meds. Make everyone see a doctor. Then maybe they’ll learn to respect medicine.
Until then, it’s just a waiting game until someone dies from a drug they thought was "harmless."
Kevin Lopez
January 13, 2026 AT 19:36Acetaminophen = liver killer. NSAIDs = gut wreckers. Diphenhydramine = dementia fuel for seniors. That’s it. No more fluff. Read the label or die. Simple.
Stop pretending this is complicated. It’s not. You just don’t care enough to learn.
Duncan Careless
January 15, 2026 AT 04:49I’m from the UK and we’ve had OTC switches for decades. The key difference? Pharmacists here are trained to ask questions. If you buy more than two packs of painkillers in a month, they’ll ask why. They’ll check your meds. They’ll warn you.
We need that model here. Not more labels. More human interaction. A pharmacist who gives a damn is worth 100 warning stickers.
Samar Khan
January 17, 2026 AT 01:38OMG I JUST REALIZED I’VE BEEN TAKING BENADRYL AND SUDAFED TOGETHER FOR MONTHS 😭😭😭
That’s why I’ve been having panic attacks and my heart feels like it’s gonna explode. I’m going to the ER right now. Thank you for this post. I thought I was just stressed. I’m not. I’m poisoned. 💔