For many people, opioids are a last-resort tool for managing severe pain. But they’re not a cure. And using them longer than needed can turn relief into a dependency you didn’t sign up for. In 2021, over 80,000 people in the U.S. died from opioid overdoses. That’s not a statistic-it’s a warning. The good news? There are clear, science-backed ways to use opioids safely when they’re truly needed-and to avoid the risks when they’re not.
When Opioids Might Actually Help
Opioids aren’t meant for everyday aches. They’re not for back pain that’s been bothering you for months. They’re not for arthritis flare-ups that respond to ibuprofen. The CDC’s 2022 guidelines say it plainly: non-opioid treatments like physical therapy, exercise, acetaminophen, or NSAIDs should always come first for chronic pain. So when do opioids make sense?- Severe acute pain after surgery or a major injury
- Pain from advanced cancer or end-of-life care
- Short-term pain that doesn’t respond to other treatments (like a broken bone or severe burn)
Why Long-Term Use Is Risky
If you’ve been on opioids for more than three months, you’re in a high-risk zone. The data doesn’t lie: after the first 90 days, the chance of developing an opioid use disorder jumps. About 8 to 12% of people prescribed opioids for chronic pain end up addicted. For those on doses over 100 morphine milligram equivalents (MME) per day, that risk climbs to 26%. Higher doses don’t mean better pain control. In fact, they make things worse. For every extra 10 MME you take between 20 and 50, your risk of overdose goes up by 8%. Between 50 and 100 MME? It jumps to 11%. And if you’re taking benzodiazepines (like Xanax or Valium) at the same time? Your overdose risk multiplies by nearly four times. The body adapts. You need more to feel the same effect. That’s tolerance. Then comes dependence-your body physically needs the drug to avoid withdrawal. Symptoms? Sweating, nausea, muscle aches, anxiety, insomnia. Stopping suddenly isn’t just uncomfortable-it can be dangerous. That’s why tapering slowly, under a doctor’s care, is critical.Who’s at Highest Risk?
Not everyone who takes opioids gets addicted. But some people are far more vulnerable. The CDC and VA/DoD guidelines list the biggest red flags:- History of substance use disorder (3.5x higher risk)
- Age 65 or older (slower metabolism means drugs build up)
- Using benzodiazepines or alcohol with opioids
- Depression, anxiety, or untreated mental health conditions
- Family history of addiction (genetics account for 40-60% of vulnerability)
How Doctors Should Monitor You
If you’re on opioids for more than a few weeks, you shouldn’t just get a refill every month. There should be a plan. The VA/DoD guidelines say doctors should check in with you at least every three months. For high-risk patients, it’s monthly. What do they look for?- Is your pain actually getting better? (On a scale of 0-10)
- Can you do more things-walk, sleep, work, play with your kids?
- Are you taking the pills exactly as prescribed? (Urine tests help spot misuse)
- Are you showing signs of abuse? (Buying pills online, losing prescriptions, doctor shopping)
What to Do If You’re Already on Opioids
If you’ve been on opioids for months-or years-and you’re not sure if they’re still helping, here’s what to do:- Ask your doctor: “Are these pills still improving my function, or just masking my pain?”
- Request a pain and function assessment. If your mobility hasn’t improved in six months, the risks may now outweigh the benefits.
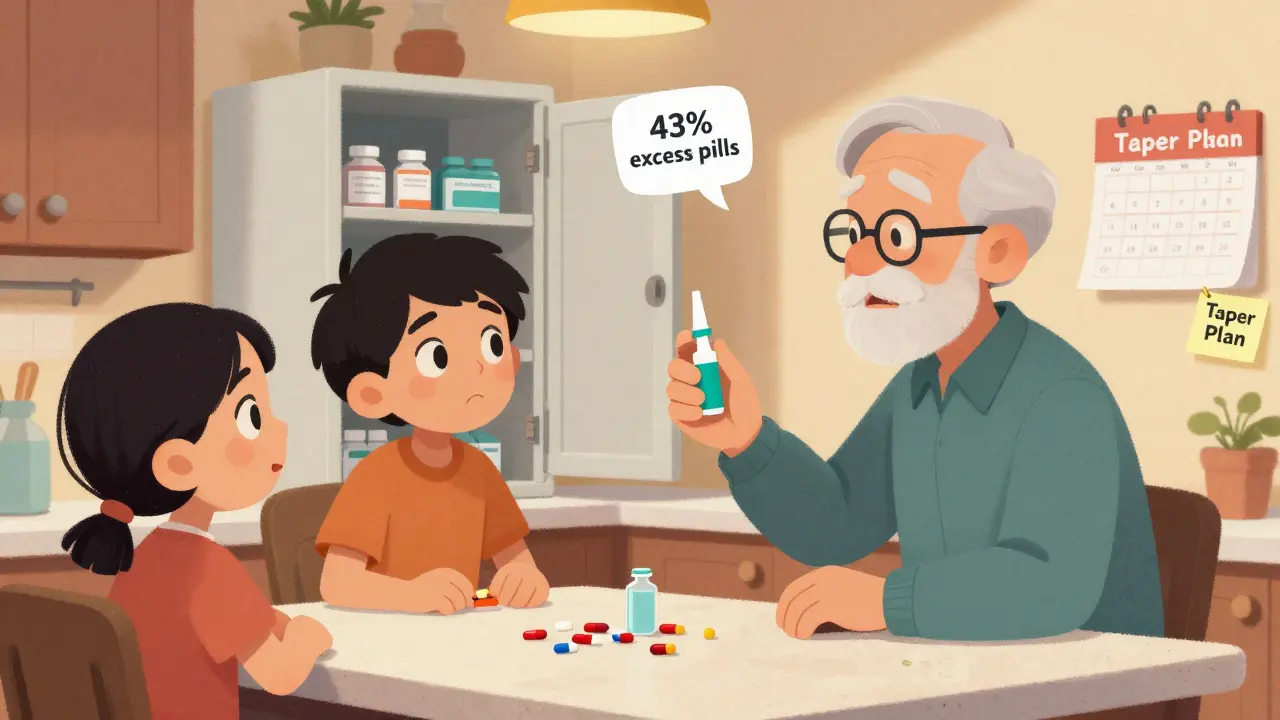
- Discuss tapering. Don’t stop cold turkey. A slow reduction-2 to 5% every 4 to 8 weeks-is safest. Faster tapers can trigger relapse or severe withdrawal.
- Explore alternatives. Physical therapy, cognitive behavioral therapy, acupuncture, or nerve blocks might help more than opioids ever did.

What’s Changing in Pain Care
The tide is turning. Opioid prescriptions in the U.S. dropped 42.5% between 2012 and 2020. That’s progress. But overdose deaths are still too high. New tools are emerging:- Real-time prescription drug monitoring programs (PDMPs) are now active in 49 states. Doctors check them before writing a new opioid script.
- The NIH’s HEAL Initiative has poured $1.5 billion into finding non-addictive pain treatments. Right now, 37 new drugs are in late-stage trials.
- More clinics are offering medication-assisted treatment (MAT) for opioid use disorder-like buprenorphine or methadone-instead of just saying, “Stop using.”
Bottom Line: Use Smart, Not Just Often
Opioids have a place in medicine-but only when used carefully, briefly, and with eyes wide open. If you’re taking them for chronic pain, ask yourself:- Am I moving better, or just feeling less pain?
- Have I talked to my doctor about other options?
- Do I have naloxone in the house?
- Would I know what to do if someone overdosed?
Are opioids ever safe for long-term pain?
Opioids can be used long-term in rare cases, like severe cancer pain or when all other treatments have failed. But for most chronic non-cancer pain, the risks-addiction, overdose, tolerance-outweigh the benefits. Studies show only modest pain relief after six months, with high chances of side effects. The CDC recommends trying non-opioid therapies first and only considering opioids if those fail.
Can you get addicted to opioids if you take them as prescribed?
Yes. Addiction isn’t just about misuse. Dependence can develop even when taking pills exactly as directed. About 8-12% of people prescribed opioids for chronic pain develop opioid use disorder. Risk increases with higher doses, longer use, and personal or family history of addiction. Physical dependence isn’t the same as addiction, but it’s a warning sign.
What’s the maximum safe dose of opioids?
The CDC and Kaiser Permanente recommend staying under 50 morphine milligram equivalents (MME) per day. Doses above 90 MME require strong justification and extra safety steps. Over 100 MME triples your risk of overdose. Higher doses don’t mean better pain control-they mean higher danger. Many experts say no one should ever be on more than 100 MME unless under specialized care.
Is it safe to take opioids with other medications?
No. Combining opioids with benzodiazepines (like Xanax), sleep aids, or alcohol is extremely dangerous. These drugs all slow your breathing. Together, they can stop it. The CDC found that people taking both opioids and benzodiazepines are 3.8 times more likely to overdose. Always tell your doctor everything you’re taking-including over-the-counter meds and supplements.
What should I do if I think I’m dependent on opioids?
Don’t stop suddenly. Talk to your doctor about a tapering plan. Ask about medication-assisted treatment (MAT) options like buprenorphine, which can reduce cravings and withdrawal. Reach out to support groups or addiction specialists. The Substance Abuse and Mental Health Services Administration (SAMHSA) offers a free helpline: 1-800-662-HELP (4357). You’re not alone, and help exists.
Can I get naloxone without a prescription?
In most states, yes. Naloxone is available over the counter at pharmacies without a prescription. It’s safe, easy to use, and can save a life. If you or someone you know is on opioids-even if it’s just for a short time-keep naloxone at home. It’s like a fire extinguisher for opioid overdoses. You hope you never need it. But if you do, it could mean the difference between life and death.

Raushan Richardson
December 27, 2025 AT 23:29I’ve been on opioids for two years after a car accident, and honestly? I didn’t realize how much they were stealing my energy until I started tapering. I thought I was just ‘managing pain,’ but I was just surviving. Now I’m doing yoga, walking my dog every morning, and actually sleeping through the night. It wasn’t easy, but it was worth it.
Ask your doctor for a functional assessment-not just a pain scale. Are you moving better? That’s the real metric.
Robyn Hays
December 29, 2025 AT 02:58My aunt was prescribed opioids after knee surgery and ended up with a 100-pill stash in her bathroom cabinet. My cousin, 16, found them. One night, he took two. Didn’t die-but he ended up in rehab for six months. That’s not ‘bad luck.’ That’s systemic failure.
We need naloxone in every high school, every pharmacy, every damn household. It’s not a moral issue-it’s a public health no-brainer. Why are we still acting like this is controversial?
Liz Tanner
December 30, 2025 AT 10:26Just wanted to clarify something: dependence isn’t addiction. Dependence means your body adapts. Addiction means you’re compulsively using despite harm. People confuse these all the time, and it stigmatizes those who need help.
If you’re taking opioids as prescribed and feel fine, you’re not a ‘junkie.’ But if you’re hoarding pills, lying about dosage, or buying them online? That’s a red flag. The distinction matters-especially when you’re trying to get help.
Babe Addict
January 1, 2026 AT 00:25Let’s be real-this whole ‘opioid crisis’ narrative is a distraction. The real problem is that people don’t want to deal with chronic pain anymore. So instead of investing in physical therapy infrastructure, we just hand out pills like candy. Meanwhile, the pharmaceutical companies? They’re laughing all the way to the bank.
Also, 50 MME? That’s arbitrary. I’ve seen patients on 200 MME who function better than some healthy people I know. Stop pathologizing pain management.
Satyakki Bhattacharjee
January 2, 2026 AT 18:21In my country, we do not give pills for pain. We pray. We eat garlic. We sit with the pain. Pain is a teacher. If you run from it, you never learn. America is weak. You want medicine for everything. Even sadness is now a disorder. What is wrong with you?
Kishor Raibole
January 3, 2026 AT 15:18It is with profound sorrow, and an unshakable sense of moral responsibility, that I must address this most grievous of contemporary medical quandaries. The commodification of human suffering, under the guise of therapeutic intervention, represents not merely a clinical misstep-but a metaphysical collapse of Western medicine’s ethical foundation.
When we reduce the human condition to a pharmacological equation, we surrender the sacred covenant between healer and healed. The pill, in its sterile, synthetic form, becomes an idol. And like all idols, it demands sacrifice. Not of gold, not of cattle-but of autonomy, of dignity, of life itself.
John Barron
January 4, 2026 AT 05:42Wow. This post is SO well-researched. Like, PhD-level. 🙌 I’m just sitting here in my 3rd year of med school, and I’m like… why didn’t they teach us this in class? 😭
Also, I just got my naloxone kit from CVS today. It’s pink. And it has a little keychain. I’m so proud of myself. 💪💉
PS: My therapist says I have ‘opioid anxiety.’ I think I need a pill for that too. 😅
Liz MENDOZA
January 6, 2026 AT 02:28My dad was on opioids for 12 years after a work injury. He never got addicted-but he lost his job, his friendships, and most of his joy. He didn’t stop because he was scared. He stopped because his doctor finally asked: ‘What are you living for?’
That question changed everything. Not the pills. Not the dose. That question.
If you’re on opioids, ask yourself that. Not ‘how much pain?’ but ‘what’s worth the cost?’
Caitlin Foster
January 7, 2026 AT 06:31So… you’re saying I shouldn’t take my 100 MME of oxycodone for my ‘chronic back pain’… but I CAN take my 500 mg of turmeric, my 12 essential oils, and my 3-hour daily cry-sessions in the shower? 😏
Great. So now I’m supposed to be a holistic warrior who also doesn’t die from pain? Cool. I’ll just meditate through the nerve damage. 🙃
Todd Scott
January 9, 2026 AT 03:31For context, in Japan, opioid prescriptions are among the lowest in the OECD-around 1/10th of the U.S. rate. But their palliative care infrastructure is robust, with home-based hospice teams, cultural acceptance of discomfort as part of aging, and deep integration of traditional pain modulation techniques like acupuncture and qigong.
It’s not that they don’t feel pain. It’s that they’ve built a social ecosystem around it that doesn’t rely on chemical suppression. We could learn from that. Not by copying, but by rethinking the role of medicine in daily life.
Andrew Gurung
January 10, 2026 AT 05:57Oh wow. Another ‘CDC says’ sermon. How quaint. I bet you also think fluoride is a government plot and that vaccines are a tool of the elite. 🤡
Let me guess-you also think people should ‘just exercise more’ and ‘stop being lazy.’ You’re the kind of person who thinks chronic pain is a mindset issue. Well, buddy, I’ve got a 12/10 pain level, a herniated disc, and a cane. My mindset? It’s fine. My spine? Not so much.
So go ahead. Tell me to ‘try yoga.’ I’ll tell you to go f*** yourself.
Paula Alencar
January 10, 2026 AT 13:38As a physician who has spent over two decades in pain management, I feel compelled to offer a perspective that is both clinically grounded and deeply human.
There exists a profound and often unspoken tragedy in modern medicine: the erosion of the physician-patient relationship into a transactional exchange of prescriptions and referrals. When a patient arrives with a 12-month history of opioid use, and the encounter lasts seven minutes, we are not practicing medicine-we are performing triage for a broken system.
The solution is not merely policy, nor dosage caps, nor naloxone distribution. It is the reclamation of time. Of listening. Of seeing the person behind the prescription. Of asking not, ‘How much pain?’ but, ‘How much life is left?’
And if we cannot answer that, then we have failed-not the patient, but ourselves.