When a patient picks up a prescription, they don’t just see a pill. They see a color, a shape, a size, a brand name they recognize-or the unfamiliar look of a generic version. For many, that difference isn’t just about cost. It’s about trust. And for people from diverse cultural backgrounds, that trust can be shaped by beliefs passed down for generations, religious rules, language barriers, or past experiences with the healthcare system.
Why a Generic Pill Doesn’t Look the Same-And Why It Matters
Generic medications contain the same active ingredient as brand-name drugs. That’s the law. But the rest? The color, the shape, the capsule shell, the fillers-they’re often completely different. That’s because generic manufacturers don’t have to copy the brand’s appearance. And that’s where problems start.In the U.S., 70% of prescriptions filled are for generics. But studies show that African American and Hispanic patients are significantly more likely to believe generics are less effective than brand-name drugs. A 2022 FDA survey found 28% of African American patients doubted generics, compared to just 15% of non-Hispanic White patients. Why? Because in many cultures, the way a medicine looks tells you whether it’s real, strong, or safe.
One pharmacist in Chicago told a story about a patient from Guatemala who refused to take her new generic blood pressure pill because it was white and oval. Her old pill was blue and round. She said, ‘If it looks different, it’s not the same medicine.’ She didn’t trust the system. She didn’t trust the pharmacist. And she stopped taking it.
Religious and Cultural Restrictions in Medication Ingredients
The active ingredient might be the same, but the inactive ingredients-called excipients-are where culture crashes into chemistry.Some capsules are made with gelatin, often derived from pigs. For Muslims, that’s haram. For Jews, it’s not kosher. For some Hindus and vegetarians, animal-derived ingredients are unacceptable. Yet most generic drug labels don’t list excipients clearly. A 2023 FDA review found only 37% of U.S. generic package inserts include detailed information about fillers, compared to 68% in the EU.
Pharmacists in cities like Detroit, Toronto, and London report getting questions about gelatin, alcohol-based preservatives, or lactose fillers at least once a week. One pharmacist spent two hours calling manufacturers just to find a liquid version of a diabetes medication without gelatin. Another had to source a halal-certified version of an antidepressant because a patient refused to swallow a capsule that might contain pork.
These aren’t rare cases. A 2023 study in the Journal of Community Pharmacy found that 63% of urban pharmacists receive these kinds of requests weekly. But most pharmacies don’t have the tools to answer them quickly. No database. No training. Just guesswork.

Color, Shape, and Cultural Meaning
Color isn’t just for branding. It carries meaning.In some East Asian cultures, white pills are associated with death or mourning. In parts of Latin America, green pills are seen as natural or herbal-sometimes trusted more than synthetic-looking ones. In West Africa, red is linked to strength and vitality. In Western cultures, blue is calming, yellow is cheerful. But if a generic pill is the wrong color, patients think it’s weak-or fake.
One study in Toronto found that elderly South Asian patients refused to take a generic version of their cholesterol medicine because it was now yellow instead of orange. They believed the color change meant the drug had lost its power. The pharmacist had to explain the science, show them the active ingredient label, and even get them a different generic version with a more familiar color.
These aren’t irrational fears. They’re learned responses. When patients have been mistreated, ignored, or misled by the healthcare system, they rely on what they can see. And if the pill looks different, they assume the medicine is different too.
The Language Gap and Patient Education
If the instructions are in English and the patient speaks only Spanish, Somali, or Mandarin, they’re not just confused-they’re at risk.Many generic medications come with printed leaflets in English only. Even when translated, the translations are often done by machines or volunteers-not trained medical interpreters. Terms like ‘take on an empty stomach’ or ‘avoid alcohol’ get lost in translation. One Cambodian patient took her generic blood thinner every morning with rice porridge because the label said ‘take with food’-but she didn’t know ‘food’ meant anything other than rice.
Pharmacies that succeed with multicultural populations don’t just hand out papers. They use visual aids: pictures of pills, videos in multiple languages, and trained cultural liaisons. Some community clinics now have ‘medication ambassadors’-bilingual staff who walk patients through their prescriptions, explain why generics are safe, and answer questions about ingredients in their native language.
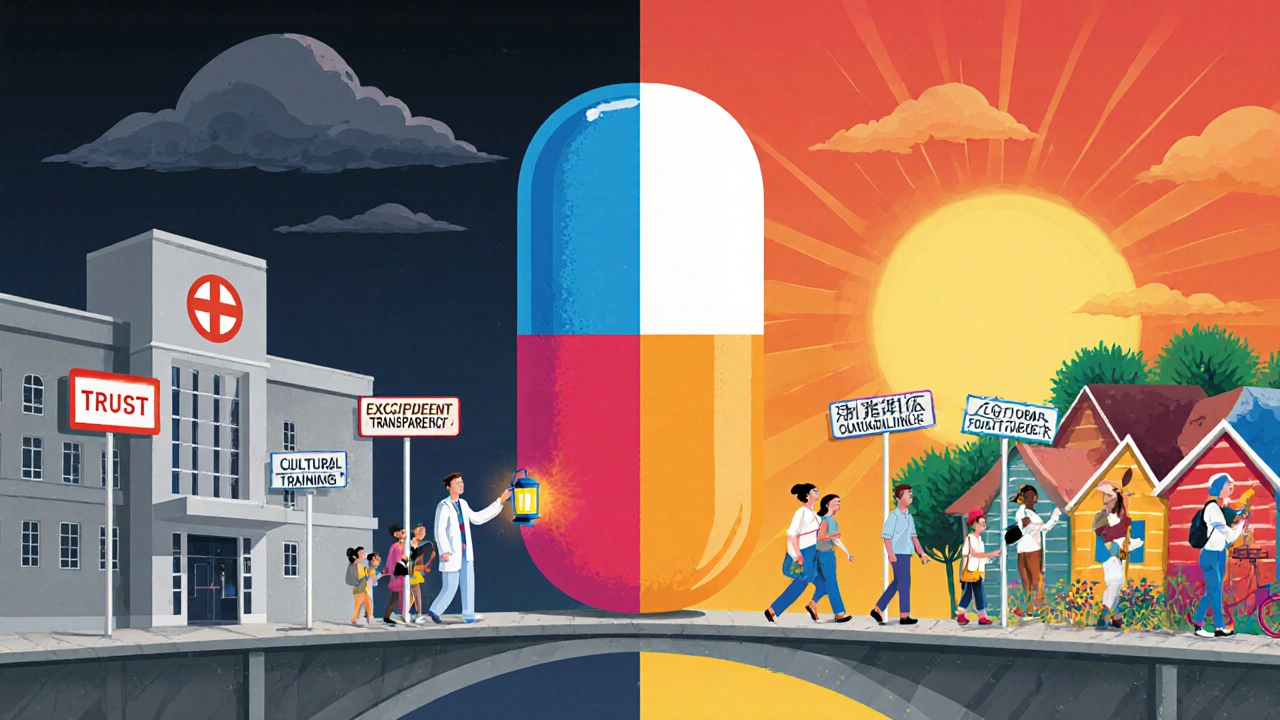
What’s Being Done-and What’s Still Missing
Change is starting, but slowly.In 2023, Teva Pharmaceutical launched a ‘Cultural Formulation Initiative’ to document all excipients in their generics across 15 major drug categories. Sandoz announced a Global Cultural Competence Framework to make this standard practice. The FDA’s Food and Drug Omnibus Reform Act (FDORA) of 2022 pushed for better inclusion of diverse populations in clinical trials and patient education.
But here’s the gap: most of this work is happening at the corporate level. Not in the pharmacy. Only 22% of community pharmacies in the U.S. have formal training on cultural considerations for generics. Most pharmacists learn by trial and error.
What’s needed isn’t just better labels. It’s:
- A public database of generic medications with excipient details (halal, kosher, vegan, allergen-free)
- Standardized visual guides showing pill shapes and colors across brands and generics
- Training for pharmacists on cultural beliefs around medicine-not just language, but meaning
- Regulatory requirements for excipient transparency in all generic drug packaging
Some chains, like CVS and Walgreens, have started pilot programs in high-diversity neighborhoods. They’ve created ‘Cultural Meds’ sections in their systems, tagging generics with flags like ‘gelatin-free’ or ‘alcohol-free.’ One pharmacy in Philadelphia reduced non-adherence by 40% in six months by simply asking patients: ‘Is there anything about this pill that makes you uncomfortable?’
It’s Not About Preference. It’s About Equity.
Generic drugs save the U.S. healthcare system over $300 billion a year. But if patients won’t take them because of cultural mistrust, those savings vanish. So do health outcomes.Chronic conditions like hypertension and diabetes hit minority communities harder. Yet those same communities are least likely to trust the generics meant to treat them. The result? Higher hospitalizations, more complications, and more deaths.
This isn’t a niche issue. It’s a systemic one. The same patient who refuses a pill because of its color might also avoid screenings because of language barriers. Or skip follow-ups because they feel misunderstood. Cultural competence isn’t a bonus. It’s a requirement for safe, effective care.
The tools exist. The data is clear. What’s missing is the will to make it standard.
Every time a pharmacist takes five extra minutes to explain why a white pill works the same as a blue one, they’re not just filling a prescription. They’re rebuilding trust.
And trust? That’s the most powerful medicine of all.


Melvina Zelee
November 23, 2025 AT 18:23Patrick Marsh
November 25, 2025 AT 05:50Daniel Jean-Baptiste
November 25, 2025 AT 13:39Miruna Alexandru
November 27, 2025 AT 13:23Latonya Elarms-Radford
November 27, 2025 AT 19:01Ravi Kumar Gupta
November 29, 2025 AT 10:58Julie Pulvino
November 30, 2025 AT 08:01Shawn Daughhetee
December 2, 2025 AT 06:28Justin Daniel
December 3, 2025 AT 01:24Holly Schumacher
December 4, 2025 AT 21:11ann smith
December 6, 2025 AT 12:37Nikhil Chaurasia
December 7, 2025 AT 08:54Mark Williams
December 8, 2025 AT 14:44