AUD Medication Selector
Find the Right Medication for You
This tool helps identify which AUD medication may be most appropriate based on your drinking patterns, goals, and medical history.
Recommended Medication
Select your options and click "Find My Match" to see your recommendation.
Important Safety Information
Never drink alcohol while taking any AUD medication. Even small amounts can reduce effectiveness and increase relapse risk. Always consult your doctor before starting or stopping medication.
When someone is trying to stop drinking, the right medication can make all the difference. But here’s the thing: even with proven treatments like naltrexone, acamprosate, or disulfiram, many people still end up back in old patterns. Why? Because medication alone doesn’t fix the problem. And when you mix these drugs with alcohol-even a little-it can undo months of progress, or worse.
How AUD Medications Actually Work
Not all medications for alcohol use disorder work the same way. That’s why choosing the right one matters.
Naltrexone blocks the brain’s opioid receptors. When you drink, alcohol usually triggers a dopamine rush that feels rewarding. Naltrexone dulls that high. It doesn’t make you sick-it just makes drinking feel less satisfying. Studies show it reduces heavy drinking days by about 5% compared to placebo. It’s especially helpful if you’re trying to cut back, not necessarily quit cold turkey.
Acamprosate works differently. After quitting alcohol, your brain chemistry gets scrambled. Glutamate and GABA systems go haywire, causing anxiety, insomnia, and cravings. Acamprosate helps rebalance those signals. It’s not a quick fix. You need to be alcohol-free for at least 3-5 days before starting it. People who stick with it for a year are more likely to stay sober.
Disulfiram is the old-school option. It doesn’t reduce cravings. Instead, it punishes drinking. If you take it and then drink alcohol, your body can’t break it down properly. You get a nasty reaction: flushing, vomiting, racing heart, even low blood pressure. It’s designed to scare you off alcohol. But here’s the catch: if you don’t take it every day, or if you think you can outsmart it, the risk of relapse goes up. Many people stop taking it because they can’t handle the fear-or because they don’t want to be constantly watching what they drink.
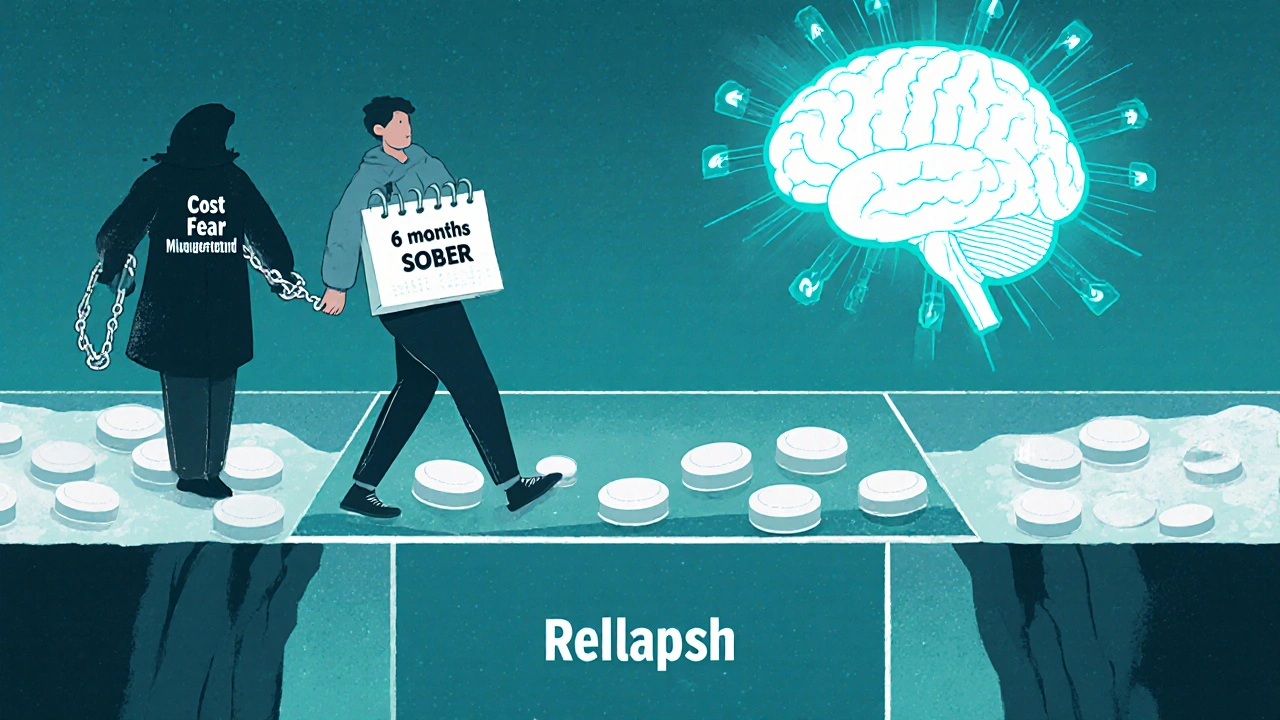
Why Relapse Still Happens-Even With Medication
Let’s be real: taking a pill every day is hard. Especially when life gets messy.
A 2023 study tracked 1,200 people on AUD medications for six months. Only 35% were still taking their meds after 90 days. Why? Side effects. For acamprosate, diarrhea and nausea pushed some people out. For naltrexone, a few felt dizzy or had stomach upset. But the biggest reason? Cost. Even though most of these drugs are generic, monthly prices still range from $20 to $400. Insurance doesn’t always cover them fully. If you’re juggling rent, food, and bills, medication becomes a luxury you can’t afford.
Then there’s the psychological trap. People think, “I’ve been sober for three months-I’m fine now.” So they stop the meds. But AUD is a chronic condition, like diabetes or high blood pressure. Stopping treatment doesn’t mean you’re cured. It means you’re going back to square one. One study found that people who quit naltrexone after six months had a 60% higher chance of returning to heavy drinking within the next year.
And here’s something no one talks about enough: some people start drinking again because they think the medication will protect them. “I’m on naltrexone, so I can have a beer.” But naltrexone doesn’t block all the effects of alcohol. It just reduces the reward. You can still get drunk. You can still lose control. And when you do, your brain remembers: alcohol = relief. That’s how relapse starts.
What Happens When You Drink While on These Medications
Drinking while on medication isn’t just risky-it can be dangerous.
If you’re on disulfiram and drink even a sip of alcohol, you’re risking a medical emergency. Symptoms can start within 10 minutes and last hours. In rare cases, it can cause heart rhythm problems or seizures. Emergency rooms see this more often than you’d think-especially among people who thought they could handle “just one drink.”
With naltrexone, drinking won’t make you sick, but it won’t help either. The drug is designed to reduce cravings and heavy drinking. If you’re drinking regularly, the medication isn’t working. You’re just wasting time and money. Worse, you’re training your brain to associate drinking with normalcy again.
Acamprosate is safer in this regard. It doesn’t interact dangerously with alcohol. But if you drink while taking it, you’re defeating the whole point. The drug helps your brain recover after quitting. If you keep drinking, your brain never gets the chance to heal. And the longer you delay healing, the harder it is to quit later.
And then there’s gabapentin, which isn’t FDA-approved for AUD but is commonly prescribed off-label. It’s especially helpful for people with a history of severe withdrawal. But if you drink while on gabapentin, you increase your risk of dizziness, confusion, and respiratory depression-especially if you’re also taking opioids or benzodiazepines.

Who Benefits Most From Each Medication?
There’s no one-size-fits-all solution. Your history, your body, and your goals matter.
- If you want total abstinence and have already detoxed, acamprosate is your best bet. It’s the most effective for long-term sobriety.
- If you’re trying to cut down on heavy drinking but aren’t ready to quit completely, naltrexone gives you more control. It reduces the urge to binge.
- If you’re highly motivated, have a strong support system, and can commit to daily dosing, disulfiram might work. But only if you’re willing to live with the fear of a reaction.
- If you have liver disease from years of drinking, gabapentin is often preferred. It’s easier on the liver than naltrexone and doesn’t require detox before starting.
A 2022 trial found that patients with high withdrawal symptoms during detox were nearly twice as likely to stay sober on gabapentin than on placebo. But for those with mild symptoms, gabapentin offered no real advantage. That’s why personalized treatment matters. One size doesn’t fit all.
The Big Problem: Underuse and Misunderstanding
Over 14 million Americans have alcohol use disorder. Only about 8% get any medication for it.
Why? Doctors don’t prescribe it. Many primary care providers don’t feel trained to handle AUD. They don’t know the differences between naltrexone and acamprosate. They don’t know how to monitor liver enzymes or adjust doses for kidney problems. And patients? They think medication is a crutch. Or they’ve heard horror stories about disulfiram reactions. Or they believe recovery means “going it alone.”
But here’s the truth: medication isn’t replacing willpower. It’s supporting it. Think of it like insulin for diabetes. You still have to manage your diet and lifestyle. But the drug gives your body a fighting chance.
And the cost of not treating AUD? It’s staggering. A 2021 study estimated that if just half of eligible patients got medication, the U.S. would save $12.7 billion a year in emergency visits, liver transplants, and lost productivity.
What You Can Do Right Now
If you’re on AUD medication:
- Don’t skip doses-even if you feel fine. Consistency is what keeps your brain stable.
- Avoid alcohol completely. Even one drink can trigger a relapse cycle.
- Track your cravings. Use a journal or app. Notice patterns: stress? loneliness? certain places?
- Get liver and kidney tests done every 3-6 months, especially if you’re on naltrexone or acamprosate.
- Ask your doctor about extended-release options. The monthly naltrexone shot (Vivitrol) improves adherence. New 6-month implants are coming soon.
- If cost is an issue, ask about generic versions or patient assistance programs. Most insurers cover these drugs now.
If you’re thinking about starting medication:
- Be honest with your doctor about your drinking habits. No judgment. Just facts.
- Ask: “Which medication fits my goals?” Not “Which one is best?”
- Plan for support. Medication works best with counseling, AA, or peer groups.
- Don’t wait until you’ve hit rock bottom. Early intervention saves lives.
What’s Next for AUD Treatment
The future is personalization.
Researchers are now using brain scans to predict who will respond to acamprosate. They’re testing blood markers and genetic profiles to match patients with the right drug. One machine learning model got it right 82% of the time.
New drugs are on the horizon. Ketamine infusions showed a 41% drop in relapse in a small 2022 trial. Microbiome treatments-like probiotics and NAC-are showing promise in early studies. And digital tools? Apps that track cravings and send real-time coping tips reduced relapse by 33% in a 2023 Lancet study.
But none of this matters if people don’t get access to the treatments we already have.
The best medication in the world won’t help if you’re afraid to take it. Or if you can’t afford it. Or if no one explained how it works.
Recovery isn’t about being perfect. It’s about staying connected-to your treatment, your support system, and your reason for wanting to change.
Medication isn’t the end of the journey. It’s the first step.
Can I drink occasionally while taking naltrexone?
No. Naltrexone reduces the rewarding effects of alcohol but doesn’t eliminate them. Drinking while on naltrexone can still lead to intoxication, poor decision-making, and increased cravings. It also makes the medication less effective over time. Even one drink can restart the cycle of dependence.
Is disulfiram safe if I have liver problems?
No. Disulfiram is processed by the liver and can cause serious liver damage, especially in people with existing liver disease. It’s generally avoided in patients with cirrhosis or elevated liver enzymes. If you have liver issues, gabapentin or acamprosate are safer alternatives.
How long should I take AUD medication?
Most guidelines recommend at least 6-12 months. For many, longer-term or indefinite use is needed. AUD is a chronic condition. Stopping medication too soon increases relapse risk. Studies show people who stay on naltrexone or acamprosate for over a year have significantly better long-term outcomes than those who quit early.
Why do some people stop taking acamprosate?
The most common reasons are gastrointestinal side effects like diarrhea and nausea, which affect about 10-15% of users. Also, acamprosate requires 3-5 days of complete abstinence before starting, which can be a barrier for those still drinking. Some people also find the pill burden high-three doses a day-though newer compacted tablets now reduce this to two daily.
Can I take these medications with other prescriptions?
It depends. Naltrexone can interact with opioid painkillers-never take them together. Acamprosate is generally safe with most drugs but requires kidney monitoring. Gabapentin can increase drowsiness when mixed with benzodiazepines or sleep aids. Always tell your doctor about every medication and supplement you take. Never adjust doses on your own.
Are there any new AUD medications coming soon?
Yes. Phase 3 trials are underway for a 6-month naltrexone implant, which could improve adherence dramatically. ALKS 5461 (a buprenorphine-samidorphan combo) showed a 32% reduction in heavy drinking days in 2023. Ketamine infusions and microbiome-targeted therapies are also in development. But the biggest breakthrough may be AI-driven matching systems that predict which medication works best for you based on your genetics, brain scans, and drinking history.


Gary Fitsimmons
October 29, 2025 AT 17:08Just wanted to say this post saved my life. I was about to quit meds because I thought I was 'fixed' after 4 months. Now I know it's like managing blood pressure. I'm staying on naltrexone. Thanks.
Tanuja Santhanakrishnan
October 31, 2025 AT 13:19As someone from India where AUD is still super stigmatized, this is the clearest breakdown I’ve ever seen. My cousin is on acamprosate now-finally got him to see a doctor after 8 years. You’re right, it’s not a crutch, it’s a bridge.
Raj Modi
November 1, 2025 AT 12:37While I appreciate the clinical precision of this exposition, one must also acknowledge the socio-economic determinants of treatment adherence that are only cursorily addressed. The cost barrier, while noted, is insufficiently contextualized within the broader framework of neoliberal healthcare disparities in the United States, wherein pharmaceutical access remains contingent upon insurance networks and bureaucratic gatekeeping rather than medical necessity. Furthermore, the omission of structural interventions-such as subsidized access programs or integration into primary care-is a critical lacuna in an otherwise robust analysis.
Bart Capoen
November 3, 2025 AT 08:06Biggest thing no one tells you: naltrexone doesn't make you 'immune' to alcohol. I thought I could have one beer to celebrate my 30-day streak. Ended up drinking the whole six-pack. Brain still remembered the high. Don't test it.
Billy Gambino
November 5, 2025 AT 00:12The neuropharmacological architecture of AUD pharmacotherapy reveals a fundamental epistemological flaw in the disease model: if addiction is a chronic brain disorder, then abstinence is not a cure, but a temporary homeostatic equilibrium maintained by exogenous modulation. Naltrexone doesn't 'cure' craving-it merely dampens the dopaminergic echo of reward. The real pathology lies not in the molecule, but in the ontological dislocation of the self from its embodied intentionality. We treat the symptom, not the existential rupture.
Karen Werling
November 6, 2025 AT 05:02❤️ This is so important. I’m a nurse and I’ve seen too many people stop meds because they feel ‘normal’ again. You’re not normal-you’re healing. Keep going. And yes, the $400/month is brutal. Ask for samples. Ask for help. You’re not alone.
STEVEN SHELLEY
November 6, 2025 AT 10:14THEY DON'T WANT YOU TO KNOW THIS BUT DISULFIRAM IS A GOVERNMENT CONTROL TACTIC TO KEEP DRINKERS SUBMISSIVE. THEY MAKE IT TERRIFYING SO YOU’LL BE TOO SCARED TO EVEN THINK ABOUT A BEER. ALSO THE FDA IS OWNED BY PHARMA. NALTREXONE IS JUST A PLACEBO WITH SIDE EFFECTS. I KNOW BECAUSE I WORKED AT A LAB THAT MADE IT. THEY DUMPED THE REAL DRUG AND SOLD THE WATER VERSION. CHECK THE BATCH NUMBERS. THEY'RE ALL THE SAME.
Emil Tompkins
November 6, 2025 AT 11:23So let me get this straight… you’re telling me I’m supposed to take a pill every day to not drink… but I’m not allowed to drink even one? What’s the point? If I’m going to be miserable either way, why not just drink and be done with it? This whole thing is just guilt-tripping people into being perfect. And now they want to implant chips? What’s next, mandatory therapy via smartwatch?
Kevin Stone
November 7, 2025 AT 22:11People who take medication for AUD are just avoiding the real work. Recovery isn't about pills. It's about facing your trauma. If you need a chemical crutch, you're not ready. I’ve been sober 12 years. Never took a pill. Just prayed and showed up. You want real recovery? Stop outsourcing your willpower.
Natalie Eippert
November 9, 2025 AT 05:59As an American taxpayer, I find it outrageous that we are subsidizing lifelong pharmaceutical dependency for a lifestyle choice. Alcohol use disorder is not a medical condition-it is moral weakness dressed up as science. Why not just tell people to stop drinking instead of spending billions on pills that don’t work? This is socialism for addicts.
kendall miles
November 9, 2025 AT 10:51Here’s the thing no one in the US will admit: the whole AUD medication model was designed by Big Pharma to replace AA. In New Zealand, we don’t have this. We have community circles, Maori healing practices, and talking. No pills. No apps. No implants. People heal when they feel connected-not when they swallow a capsule. Your system is broken.
Cecil Mays
November 10, 2025 AT 07:09Just got my Vivitrol shot today. First time in 6 years I didn’t have to think about taking a pill every day. I’m crying. Not because I’m healed-but because I finally feel like I can breathe. Thank you for writing this. You didn’t just explain meds-you explained hope.
Sarah Schmidt
November 12, 2025 AT 04:52There’s a profound irony in framing addiction as a chronic disease while simultaneously demanding perfect compliance with pharmaceutical regimens-this is not medicine, it’s behavioral conditioning dressed in scientific garb. The very notion that a pill can resolve existential dissonance betrays a Cartesian dualism that reduces the soul to a neurotransmitter equation. One wonders whether we are treating illness-or manufacturing dependency to sustain an industry.
Bob Martin
November 12, 2025 AT 18:41So you’re telling me I can’t have a beer on naltrexone… but I can have 12 shots of tequila? Just kidding. But seriously, why does everyone act like this is some miracle cure? I’ve been on it for 8 months. I still wake up wanting a drink. The pill doesn’t fix your life. It just gives you a little more time to figure it out.
Glenda Walsh
November 13, 2025 AT 02:58Wait-so if I drink while on acamprosate, it doesn’t make me sick? But it still doesn’t help? Then why am I paying $300 a month for a placebo that makes me poop? I’m done. I’m going back to AA. At least there, they don’t charge me for hope.