When you’ve been on the same psychiatric medication for months-or even years-it stops feeling like a pill. It becomes part of you. A quiet anchor. Then one day, your doctor says, "Let’s switch." Maybe it’s because it’s not working well enough. Maybe your insurance dropped the brand. Maybe they switched you to a generic without telling you. Suddenly, you’re not just changing a drug. You’re changing your mind.
It’s Not Just the Chemistry
People assume switching medications is like swapping one pair of shoes for another. If they’re both size 9, it should work fine. But with psychiatric drugs, it’s not about size. It’s about how your brain has adapted. Your neurons have rewired around that chemical. You’ve built routines, coping strategies, even emotional rhythms around it. When you pull that out, even slowly, your brain doesn’t just adjust-it stumbles. A 2023 study from King’s College London tracked over 40,000 people on antidepressants. About 11% switched within 90 days. That’s not rare. That’s normal. But here’s what they found: switching didn’t just mean a new dose. It meant a new emotional landscape. Many described feeling like they’d lost a version of themselves. One participant said, "I didn’t feel sad anymore. I just felt… empty. Like I was watching my life through glass." This isn’t just anecdotal. The American Psychiatric Association officially recognized medication discontinuation syndromes in the DSM-5 back in 2013. That means they’re not just "side effects." They’re clinical phenomena. Electric-shock sensations. Dizziness. Brain zaps. Insomnia that feels like your nerves are frayed. These aren’t minor inconveniences. They’re neurological tremors caused by sudden chemical shifts.Generic Switches Are the Silent Trigger
The biggest surprise? The problem isn’t always brand versus generic. It’s switching formulations at all. A 2019 review by Dr. Pierre Blier found that 68% of bad reactions happened when patients were switched from one generic version to another-same active ingredient, same dosage, same manufacturer, just a different pill shape or filler. Your body doesn’t care about the label. It cares about how fast the drug enters your bloodstream. Even tiny differences in absorption can throw off your brain’s delicate balance. One patient on PatientsLikeMe switched from brand-name sertraline to a generic and spent three weeks feeling emotionally numb. Then came panic attacks-something she hadn’t had in two years. She ended up in the ER. Another Reddit user wrote: "I was stable for 18 months. They switched me to a cheaper generic. Two weeks later, I couldn’t get out of bed. My therapist said I was relapsing. I told her I hadn’t changed anything except the pill. She didn’t believe me." That’s the cruel part. When you report these symptoms, you’re often told you’re "not compliant," "overreacting," or "just anxious." But the science says otherwise. A 2021 meta-analysis showed that when tapering schedules matched a drug’s half-life, withdrawal symptoms dropped by 30%. Paroxetine, with its 21-hour half-life, needs a slow taper. Fluoxetine, with its 96-hour half-life, can be stopped faster. But most primary care doctors don’t know this.The Trust Erosion Effect
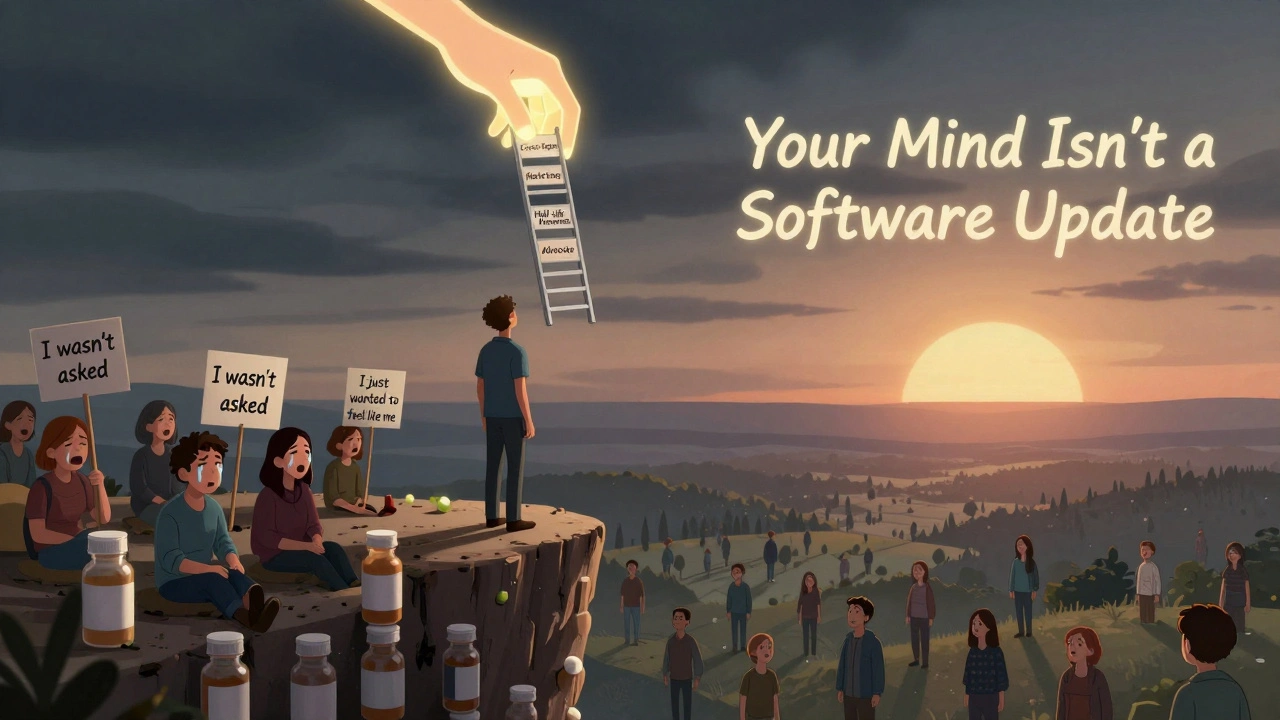
Psychological damage doesn’t stop at physical symptoms. There’s a deeper wound: loss of trust. A 2023 poll on Psych Central found that 74% of patients felt less confident in their treatment after an unplanned switch. Why? Because they weren’t asked. They weren’t warned. They were just handed a new prescription. It felt like a betrayal. Dr. K. N. Roy Chengappa, a leading psychopharmacologist, says: "Patients often feel like their care is being managed by a spreadsheet, not a person." That’s especially true when switching happens because of insurance formulary changes or cost-cutting measures. You’re not just losing your medication-you’re losing your sense of agency. This isn’t just about mental health. It’s about dignity. One man in a NAMI survey said, "I’ve been on the same meds for 12 years. I didn’t ask to be a cost-saving experiment. I just wanted to feel like myself again."
Who Gets Left Behind?
Not everyone experiences switching the same way. Socioeconomic factors play a huge role. Data from the UK Biobank shows people earning under $30,000 a year were 33% more likely to have a negative psychological reaction to a switch than those earning over $75,000. Why? Access to follow-up care. Ability to take time off work. Ability to afford copays for monitoring. Even access to a therapist who understands what’s happening. University-educated patients were 25% less likely to switch antidepressants. Not because they were healthier. Because they knew how to advocate. They asked questions. They pushed back. They requested continuity. Meanwhile, 61% of primary care providers admit they don’t feel trained enough to manage cross-tapering safely. And only 37% of electronic health records even have a built-in protocol for medication switches. That means most transitions happen in the dark.How to Switch Safely
You don’t have to accept a bad switch. Here’s what actually works:- Ask why. Don’t just sign the prescription. Ask: "Why are we switching? Is it because of my symptoms-or my insurance?"
- Request a cross-taper. Never stop cold. Never switch abruptly. A gradual overlap-reducing the old while slowly adding the new-cuts psychological side effects by 37%. It takes 2-4 weeks. That’s time well spent.
- Know your drug’s half-life. Paroxetine? Citalopram? Short half-life. Taper slow. Fluoxetine? Escitalopram? Longer half-life. You can move faster. Ask your pharmacist for this info.
- Track your symptoms. Keep a simple log: mood, sleep, energy, brain zaps, anxiety spikes. Use a notes app. Write it down daily. This isn’t fluff. It’s evidence.
- Insist on monitoring. Schedule a check-in one week after the switch. Then again at two weeks. If you’re not feeling better-or worse-by then, speak up.
When Switching Can Help
It’s not all bad. For some, switching is a lifeline. Twenty-eight percent of people in the NAMI survey reported feeling better after a switch-especially if they moved from a med that fogged their thinking to one that didn’t. Someone on sedating antipsychotics might feel clearer after switching to a newer agent. Someone on an SSRI with sexual side effects might finally feel like themselves again on bupropion. The key difference? Intention. Control. Communication. When the switch is planned, explained, and supported, the psychological toll drops dramatically.The Bigger Picture
We’re in the middle of a mental health crisis. More people are on meds than ever. More prescriptions are being written by primary care doctors than psychiatrists. And the system is stretched thin. But here’s the truth: psychiatric medications aren’t like antibiotics. You don’t just take them until the infection clears. They reshape your brain chemistry. They become part of your identity. Switching them without care isn’t just risky. It’s reckless. The FDA is starting to pay attention. Their 2022 draft guidance on complex generics now acknowledges that "bioequivalence doesn’t always mean therapeutic equivalence"-especially for CNS drugs. That’s a big deal. And in 2024, a new national surveillance system will start tracking real-world psychological outcomes from medication switches across 25 million patients. Until then, you’re your own best advocate. If you’re being switched, don’t stay silent. Ask for time. Ask for data. Ask for respect. Your mind isn’t a machine. It’s not a software update you can just reboot. It’s a living system. And it deserves more than a pharmacy label change.Can switching antidepressants cause depression to get worse?
Yes. Studies show 71% of patients who were switched without their knowledge-from brand to generic or between generics-experienced worsening symptoms or relapse. Even when the new drug is "equivalent," the act of switching itself can destabilize the brain’s chemical balance, leading to increased anxiety, emotional numbness, or full depressive episodes. This is especially true if the switch is abrupt or poorly monitored.
Why do I feel worse after switching to a generic medication?
It’s not always about the active ingredient. Generic medications can have different fillers, binders, or release mechanisms that affect how quickly the drug enters your bloodstream. Even small changes in absorption can disrupt your brain’s adaptation to the medication. Many people report "brain zaps," dizziness, or mood swings not because the drug is weaker, but because their nervous system is reacting to the change in formulation-not the drug itself.
How long does it take to adjust after switching psychiatric meds?
Adjustment varies by drug and individual. For antidepressants, most people start to stabilize within 2-6 weeks, but full adaptation can take up to 3 months. Medications with short half-lives (like paroxetine) often cause more intense withdrawal, requiring longer tapers. If symptoms worsen after 4 weeks or you have suicidal thoughts, contact your provider immediately. Waiting too long can lead to hospitalization.
Is it safe to switch medications on my own?
No. Abruptly stopping or switching psychiatric medications can trigger severe withdrawal symptoms, including seizures, extreme anxiety, hallucinations, or suicidal ideation. Even "mild" drugs like SSRIs can cause dangerous discontinuation syndromes. Always work with your prescriber. If you’re unhappy with your current med, ask for a plan-not a replacement.
What should I ask my doctor before a medication switch?
Ask: Why are we switching? Is it because of my symptoms or my insurance? What’s the plan for tapering and starting the new med? How will we monitor my response? Can we use a cross-taper? Will you check my half-life and adjust the schedule? Will you document this in my record? If they can’t answer clearly, seek a second opinion.
Are there any tests that can predict how I’ll react to a switch?
Pharmacogenetic tests (like those from Genomind) analyze how your genes metabolize certain drugs. They can show if you’re a fast or slow metabolizer, which may help predict side effects. But they’re not perfect. Only 15% of primary care providers use them regularly, and research on their ability to predict switching outcomes is still limited. They’re a tool-not a crystal ball.


Lauren Scrima
December 13, 2025 AT 12:09So… you’re telling me my brain zaps aren’t just ‘stress’? I’ve been told that for two years. Thanks for validating what my nervous system has been screaming. I’m not crazy. I’m just pharmacologically betrayed.
Hamza Laassili
December 14, 2025 AT 08:09Ugh this is why america sucks. Insurance companies run everything. I got switched to some generic crap and now i cant even focus on my job. My boss thinks im lazy. But nooo its not me its the pill they gave me. Wtf.
Rawlson King
December 15, 2025 AT 08:53There is no such thing as therapeutic equivalence in CNS drugs. The FDA’s bioequivalence standards are laughably inadequate for psychiatric medications. This is not a controversy-it is a systemic failure of regulatory science. The data is overwhelming, and yet the medical establishment continues to treat patients like lab rats.
Constantine Vigderman
December 16, 2025 AT 05:22YOU ARE NOT ALONE. Seriously. I went through this last year. Numb. Empty. Brain zaps every time I moved my head. I kept a journal like the post said. Showed it to my doc. They finally listened. Took 6 weeks to taper. Now I’m back to me. You got this. 💪
Tom Zerkoff
December 17, 2025 AT 00:51It is imperative to recognize that the pharmacokinetic variability inherent in generic formulations-particularly those with narrow therapeutic indices-poses a clinically significant risk to patients with psychiatric conditions. A standardized protocol for cross-tapering, inclusive of half-life considerations and patient-reported outcome tracking, must be integrated into primary care workflows. This is not optional. It is a matter of clinical ethics.
Yatendra S
December 18, 2025 AT 00:35Our minds are not machines. They are rivers. And when you dam them, even for a moment, the water finds a new path. Sometimes it floods. Sometimes it dries. But it never flows the same. 🌊
Himmat Singh
December 19, 2025 AT 02:41The notion that psychiatric medications are 'part of one's identity' is a dangerous anthropomorphization of pharmacological agents. The brain is plastic. Adaptation is not loss. This narrative risks reinforcing patient dependency on chemical crutches rather than promoting psychological resilience. The data does not support the emotional rhetoric presented here.
Webster Bull
December 19, 2025 AT 03:00My brain zaps felt like tiny lightning strikes inside my skull. I thought I was losing it. Turns out? Just a bad pill swap. Now I ask for the half-life before they scribble anything. Seriously. Do it. Save yourself.
Scott Butler
December 20, 2025 AT 19:02This is why we need to stop coddling people. If you can’t handle a pill change, maybe you’re not ready to be functional. Stop blaming the system. Take responsibility. Your brain isn’t fragile. You’re just weak.
Michael Gardner
December 21, 2025 AT 18:59Actually, the 11% switching rate in that King’s College study? That’s low. In my clinic, it’s closer to 30%-mostly because of insurance formularies. We’re not talking about rare cases. We’re talking about the norm. And nobody’s tracking the fallout.
Harriet Wollaston
December 22, 2025 AT 22:42I cried when I realized I wasn’t depressed-I was just reacting to a different filler. Thank you for saying this. I felt so alone. Now I’m telling everyone I know. This needs to be common knowledge.
sharon soila
December 23, 2025 AT 22:29If you are being switched, please write down how you feel every day. Even one sentence. You will be surprised how clear it becomes after two weeks. And show it to your doctor. They need to see it. You are not overreacting. You are being smart.
nina nakamura
December 24, 2025 AT 08:00Stop whining. If you can’t handle a medication change, you shouldn’t be on one. This is just pharmaceutical dependency dressed up as trauma. The system isn’t broken. You’re just addicted to feeling safe.
Cole Newman
December 25, 2025 AT 10:09Wait so you’re telling me I’m not just lazy? I thought I was failing at life. Turns out I was just on a bad generic. My therapist said I was ‘resisting change.’ I almost quit therapy. Thanks for this. I’m printing it out.