Obesity isn’t just about eating too much or not exercising enough. It’s a chronic disease-just like high blood pressure or diabetes-and it needs ongoing medical care. In 2025, the American College of Cardiology officially recognized this with new clinical guidelines that treat weight management as a medical priority, not a personal failure. Medical weight management isn’t a quick fix. It’s a structured, science-backed approach that combines clinics, medications, and regular monitoring to help people lose weight and keep it off-while improving their overall health.
What Counts as Medical Weight Management?
Medical weight management is different from commercial diet programs. It’s led by doctors, dietitians, and behavioral specialists who work as a team. These clinics don’t sell shakes or promise 20-pound losses in two weeks. Instead, they use proven methods: personalized nutrition plans, physical activity guidance, behavior change coaching, and FDA-approved medications when needed.
To qualify, you typically need a BMI of 30 or higher-or a BMI of 27 or higher if you have conditions like high blood pressure, type 2 diabetes, or sleep apnea. These aren’t arbitrary numbers. They’re based on decades of research showing that losing just 5% of your body weight can lower your blood sugar, reduce your blood pressure, and ease joint pain. Losing 10% or more? That’s when you start seeing real disease-modifying effects, like putting type 2 diabetes into remission.
How Clinics Actually Work
Most medical weight management clinics follow a clear process. First, you’ll have your BMI checked and your health history reviewed. Then, you’ll complete a pre-appointment questionnaire-sometimes through an app-that asks about your eating habits, stress levels, sleep, and what’s held you back in the past. This isn’t just paperwork. It helps your team understand your unique barriers.
Before your first visit, many clinics require you to watch a short orientation video or read a patient handbook. This sets expectations: you’re not here for a magic pill. You’re here to learn how to manage a chronic condition. Appointments usually start with a 45- to 60-minute session with a registered dietitian who builds a meal plan around your food preferences, budget, and lifestyle-not a rigid list of “good” and “bad” foods.
Follow-ups happen every 2 to 4 weeks. These aren’t weigh-ins. They’re check-ins. Your provider asks: How was your sleep? Did you feel stressed this week? Did you eat out? What worked? What didn’t? This approach, backed by the Academy of Nutrition and Dietetics, cuts long-term failure rates from over 80% down to around 40%.
The Medications: What’s Working Now
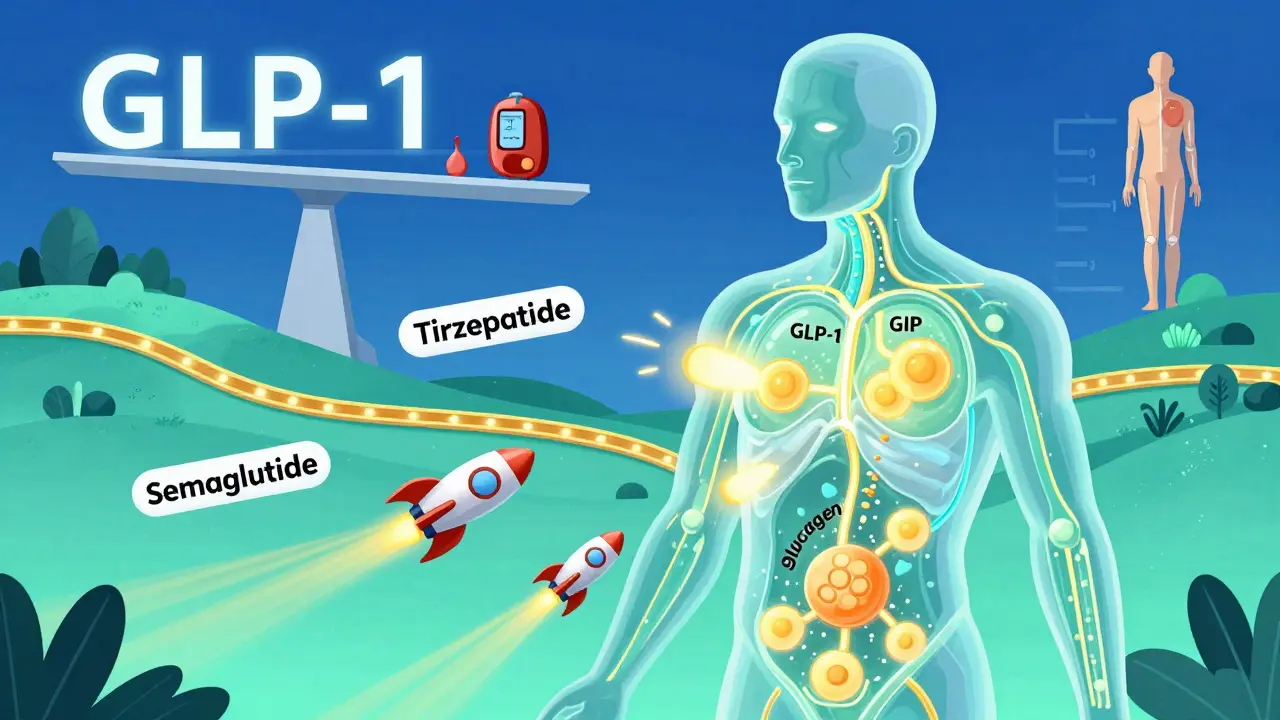
Medication isn’t a last resort-it’s a core tool. In 2025, the most effective drugs are GLP-1 receptor agonists and newer dual- or triple-agonists. Semaglutide (Wegovy®) and tirzepatide (Zepbound®) are the top choices. In clinical trials, people on semaglutide lost an average of 14.9% of their body weight over 72 weeks. Tirzepatide? That jumped to 20.2%. These aren’t theoretical numbers. Real patients in Austin, Nashville, and Chicago are seeing similar results.
There’s a new player on the scene: retatrutide. It’s a triple agonist (targeting GLP-1, GIP, and glucagon) that showed 24.2% weight loss in early trials. It’s not FDA-approved yet, but it’s already changing how doctors think about long-term treatment.
But here’s the catch: insurance coverage. Only 68% of commercial insurers cover these medications in 2025. Medicare Advantage plans? Only 12% cover them. That means many patients pay $1,000 to $1,300 a month out of pocket. Compare that to commercial diet apps that cost $20 to $60 a month-and you see why cost is the biggest barrier.
Monitoring: It’s Not Just About the Scale
Successful programs don’t just track weight. They monitor waist circumference, blood pressure, fasting glucose, liver enzymes, and even mood and energy levels. The American Diabetes Association says these checks should happen at least every three months during active treatment.
Why? Because weight loss isn’t just about looking different. It’s about feeling better and living longer. A 2024 JAMA study found that people in medical programs lost nearly twice as much weight (9.2%) as those in commercial programs (5.1%) after one year. And the health benefits? They stick. People who stick with medical management for two years are 3x more likely to keep off 10% of their weight than those who quit after six months.
Many clinics now use electronic health record templates that automatically flag obesity-related risks-something 68% of academic hospitals adopted by 2025. This ensures your weight isn’t ignored during a visit for back pain or a cold.
Why This Works Better Than Diet Programs
Commercial weight loss programs focus on calories. Medical programs focus on biology. They understand that hormones, stress, sleep, and genetics all play a role. A person with insulin resistance won’t lose weight the same way as someone with a thyroid issue. One-size-fits-all plans fail 80% of the time. Personalized care? That’s where success lives.
Patients consistently say the most helpful parts are the non-judgmental environment and the personalized meal planning. One patient on Reddit said the pre-appointment questionnaire in West Virginia University’s program helped her realize she was eating more at night because she was anxious-not hungry. That insight changed everything.
And the results speak for themselves. A 2025 survey by the Obesity Action Coalition found 78% of participants reported better quality of life after six months. Sleep improved. Joint pain dropped. Confidence went up.

The Hidden Challenges
It’s not perfect. Appointment wait times can be 4 to 8 weeks. Some clinics have long waiting lists. And even though 47% of Fortune 500 companies now offer medical weight management as a benefit, many people still don’t know it’s covered.
There’s also bias. Doctors still sometimes avoid the topic, fearing they’ll offend. The ACC guidelines now explicitly recommend: use chairs without armrests, offer blood pressure cuffs in multiple sizes, and never say, “You just need to eat less.” Language matters. So does training. Since 2023, the number of board-certified obesity medicine physicians has grown by 29%-but we still need more.
Disparities remain. Black and Hispanic patients are 43% less likely to be offered medication-even when they meet the same BMI and health criteria. This isn’t about access alone. It’s about systemic gaps in care.
What’s Next?
The future is integration. By 2030, the American Diabetes Association predicts weight management will be as routine in diabetes care as checking HbA1c levels. Primary care clinics will start offering it. Employers will expand coverage. Insurance companies will catch up.
And the data shows it’s worth it. Every $1 spent on medical weight management saves $2.87 in reduced diabetes and heart disease costs within five years. That’s not just good for patients. It’s good for the system.
If you’ve tried diets and failed, it’s not you. It’s the system. Medical weight management isn’t about willpower. It’s about science, support, and sustained care. And it’s working-for thousands of people right now.
Is medical weight management only for people with severe obesity?
No. Medical weight management is for anyone with a BMI of 30 or higher, or a BMI of 27 or higher with conditions like high blood pressure, diabetes, or sleep apnea. You don’t need to be severely overweight to benefit. Losing just 5% of your body weight can significantly improve your health.
Are GLP-1 medications like Wegovy and Zepbound safe?
Yes. These medications have been studied in tens of thousands of people and are FDA-approved for long-term use. Side effects like nausea or diarrhea are common at first but usually fade within weeks. Serious side effects are rare-far less common than with bariatric surgery, which has a complication rate of nearly 5%. Always discuss your medical history with your provider before starting.
How much does a medical weight management program cost?
Costs vary. Clinic programs typically range from $150 to $300 per month, including appointments, dietitian visits, and medication if prescribed. Commercial apps cost $20 to $60, but they lack medical oversight. Insurance coverage for medications is still patchy-only 68% of commercial plans cover them. Some employers now offer full or partial coverage as part of wellness benefits.
Can I get these medications from my regular doctor?
Some primary care doctors do prescribe them, especially if they’ve completed obesity medicine training. But many still don’t feel confident managing the treatment long-term. Specialized clinics have teams trained in nutrition, behavior, and pharmacology. For the best results, especially if you have multiple health conditions, a dedicated weight management clinic is recommended.
How long do I need to stay in the program?
Obesity is a chronic condition, so treatment is meant to be ongoing. Most people need at least 12 to 18 months of active support to build lasting habits. After that, many transition to maintenance visits every 3 to 6 months. Stopping treatment too soon often leads to weight regain. Think of it like taking blood pressure medication-you don’t stop when you feel better.
What if my insurance won’t cover the medication?
Some clinics offer patient assistance programs or coupons to lower out-of-pocket costs. Others work with pharmacies to find lower-cost alternatives or generic versions as they become available. You can also ask your employer if they offer a wellness stipend. And in some states, Medicaid is starting to cover these medications-check your local guidelines.
Do I need to follow a strict diet?
No. Medical weight management avoids rigid diets. Instead, you work with a dietitian to build flexible, sustainable eating habits. That might mean reducing sugary drinks, eating more protein, or planning meals ahead. The goal isn’t perfection-it’s consistency. You can still eat your favorite foods, just in smarter portions and frequencies.
How do I find a medical weight management clinic near me?
Start by asking your primary care provider for a referral. You can also search through the Obesity Medicine Association’s directory or check if your hospital system offers a program. Many academic medical centers, like Mayo Clinic, Cleveland Clinic, and West Virginia University Health System, have established clinics. Look for programs that include a team of physicians, dietitians, and behavioral coaches-not just a single provider.


Dan Pearson
February 2, 2026 AT 02:20Chinmoy Kumar
February 3, 2026 AT 00:55Brett MacDonald
February 3, 2026 AT 20:17Sandeep Kumar
February 3, 2026 AT 21:16Gary Mitts
February 5, 2026 AT 08:48Bridget Molokomme
February 5, 2026 AT 17:42phara don
February 6, 2026 AT 23:13Hannah Gliane
February 8, 2026 AT 15:47Murarikar Satishwar
February 9, 2026 AT 01:10Bob Hynes
February 10, 2026 AT 02:52