When your thyroid slows down, your whole body feels it. You’re tired all the time, even after a full night’s sleep. You gain weight without changing your diet. You feel colder than everyone else in the room. Your skin gets dry, your hair thins, and even simple tasks feel like climbing a hill. If this sounds familiar, you might be dealing with hypothyroidism-an underactive thyroid that’s not making enough hormones to keep your metabolism running right.
What Exactly Is Hypothyroidism?
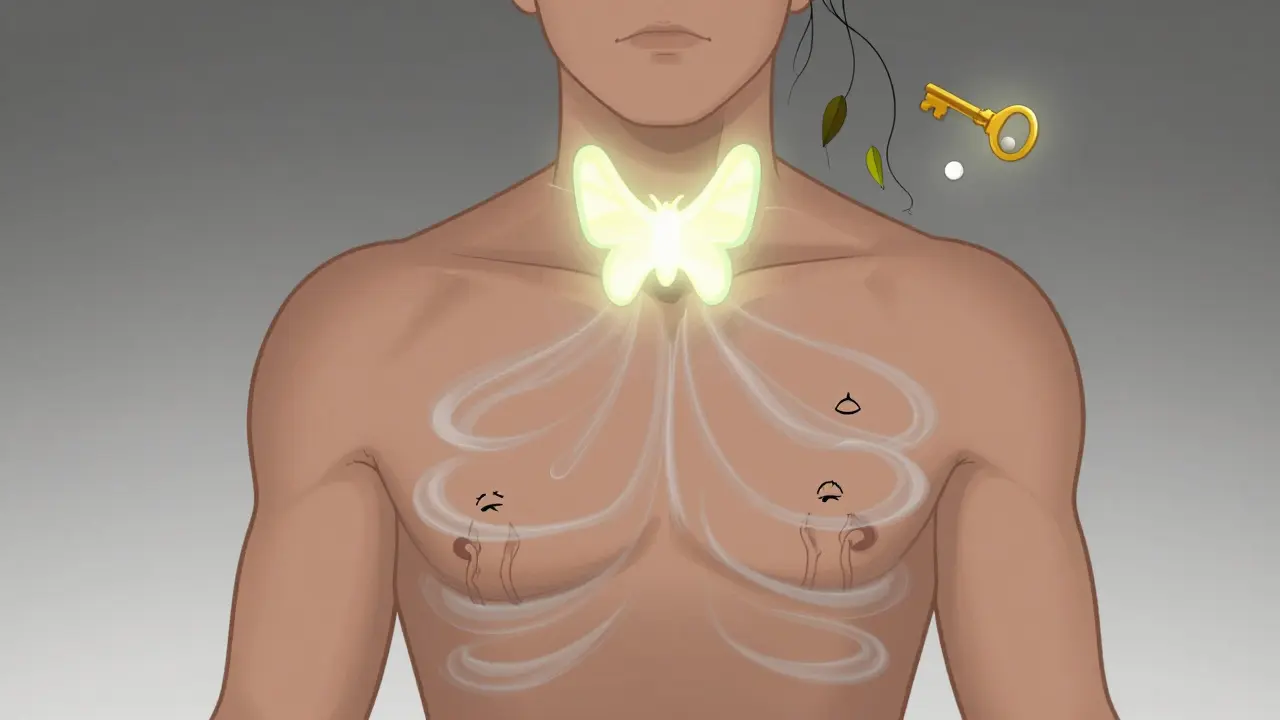
Hypothyroidism happens when your thyroid gland, a small butterfly-shaped organ at the base of your neck, stops producing enough thyroid hormones-mainly T4 (thyroxine) and T3. These hormones control how your body uses energy. When levels drop, everything slows down: your heart, your digestion, your brain, even your skin’s ability to repair itself. About 95% of cases are called primary hypothyroidism, meaning the problem starts in the thyroid itself. The other 5% are central hypothyroidism, where the pituitary gland or hypothalamus fails to signal the thyroid to work. In the UK and US, the #1 cause is Hashimoto’s thyroiditis-an autoimmune disease where your immune system attacks your thyroid by mistake. It’s not rare. In fact, up to 15% of women over 60 have it.How Do You Know You Have It?
Symptoms don’t always show up at once. Many people think they’re just getting older or stressed. But here’s what actually happens in most cases:- 95% feel constant fatigue
- 85% are unusually sensitive to cold
- 75% gain 5-10 kg without reason
- 60% struggle with constipation
- 50% notice dry skin, brittle nails, or hair loss
- 40% describe brain fog-trouble focusing or remembering things
- 30% feel depressed or low for no clear reason
How Is It Diagnosed?
The first test is always a blood test for TSH. If it’s high, your doctor will check your free T4 (FT4). In true hypothyroidism, TSH is above 4.0 mIU/L and FT4 is below 0.8 ng/dL. If TSH is high but FT4 is normal, that’s subclinical. If TSH is normal or low but FT4 is low, that’s central hypothyroidism-a rarer form. Doctors also test for thyroid antibodies, especially anti-TPO. If they’re positive, it’s almost certainly Hashimoto’s. This test is accurate in 90% of cases. Modern TSH assays are so precise that diagnosis is over 98% accurate when both TSH and FT4 are checked together.Levothyroxine: The Standard Treatment
There’s no cure for Hashimoto’s or most other causes of hypothyroidism. But there’s an excellent treatment: levothyroxine. It’s a synthetic version of T4, the hormone your thyroid should be making. Your body converts it into T3 as needed. The starting dose depends on your age, weight, and health. For most adults under 50 without heart problems, it’s about 1.6 mcg per kg of body weight. That usually means 100-150 mcg a day. For older adults or those with heart disease, doctors start low-25 to 50 mcg-and increase slowly, every 6 weeks, to avoid stressing the heart. It’s not a quick fix. You won’t feel better the next day. Most people notice more energy after 2-3 weeks. Full improvement takes 6-8 weeks. That’s why doctors wait that long before retesting TSH.How to Take Levothyroxine Right
Getting the dose right matters-but so does how you take it. Here’s what actually works:- Take it on an empty stomach, 30-60 minutes before breakfast
- Use only water-no coffee, no juice, no food
- Avoid calcium supplements, iron, or antacids for at least 4 hours after
- Don’t take it with soy milk or high-fiber meals-they cut absorption by up to 50%
- Store it in a cool, dry place. Humidity can degrade it by 15% in a month
What If You Still Feel Bad?
You’re not alone if you’re taking levothyroxine and still feel tired. About 25% of patients report persistent symptoms even when their TSH is in the “normal” range. That’s because TSH doesn’t tell the whole story. Some people don’t convert T4 to T3 well. Others have underlying inflammation or nutrient deficiencies-like low iron, vitamin D, or B12-that block thyroid hormone use. Before blaming the medication, ask your doctor to check:- Ferritin (iron stores)
- Vitamin D
- B12 and folate
- Reverse T3 (in some cases)
Special Cases: Pregnancy, Elderly, and More
Pregnant women need more thyroid hormone-often 25-50% more. TSH targets drop to under 2.5 mIU/L in the first trimester. Untreated hypothyroidism during pregnancy increases the risk of miscarriage, preterm birth, and developmental delays in the baby. That’s why all women with Hashimoto’s should have their dose checked before trying to conceive. For people over 85, the goal isn’t to get TSH down to 1.0. It’s to avoid over-treatment. Too much thyroid hormone can cause heart rhythm problems or bone loss. Doctors often aim for a TSH between 4 and 6 mIU/L in this group. Combination therapy-taking both levothyroxine and liothyronine (T3)-sounds logical. But 85% of clinical trials show no real benefit over levothyroxine alone. The American Thyroid Association doesn’t recommend it unless you’ve tried everything else and still have symptoms.What Happens If You Don’t Treat It?
Left untreated, hypothyroidism doesn’t just make you feel sluggish. It raises your risk for serious problems:- 25% develop high cholesterol, increasing heart disease risk by 30%
- 15% get peripheral neuropathy-numbness or tingling in hands and feet
- 20-30% of women struggle with infertility
- Myxedema coma, though rare, kills 20-50% of those who get it

How Often Should You Get Tested?
Once you start levothyroxine, TSH is checked every 6-8 weeks until it’s stable. Then, once a year is enough-for most people. But if you’re pregnant, change medications, gain or lose weight, or start new drugs (like estrogen or seizure meds), you’ll need testing sooner. Always get your blood drawn in the morning, before eating or taking your pill. TSH levels can drop after food or caffeine, giving false results.What About Cost and Access?
Levothyroxine is one of the cheapest medications out there. In the US, generics cost $4-$30 a month. Brand-name Synthroid runs $30-$60. In the UK, it’s available free on the NHS. If you’re paying more than £10 a month privately, ask your pharmacist about generic alternatives.What’s New in Treatment?
Research is moving beyond TSH. Scientists are testing time-release levothyroxine pills that let you take them at night without fasting-early trials show better adherence and more stable hormone levels. Genetic tests are also being developed to predict who’s at risk for Hashimoto’s before symptoms start. But here’s the bottom line: levothyroxine isn’t going anywhere. Endocrinologists agree it’s still the gold standard, and will be for at least the next five years.Real Talk: What Patients Say
A 2023 survey by the Thyroid Patient Advocate Foundation found:- 30% struggle to take their pill before breakfast because of shift work
- 40% hate waiting 6-8 weeks for a blood test to see if their dose is right
- 85% say their energy improved dramatically once their TSH was in the right range
- 90% report feeling like themselves again after 3-6 months of consistent treatment
Can hypothyroidism go away on its own?
Rarely. In some cases, like postpartum or subacute thyroiditis, thyroid function may return to normal after a few months. But for most people-especially those with Hashimoto’s-it’s permanent. Even if symptoms disappear, the underlying damage to the thyroid remains. Stopping medication leads to a return of symptoms, often worse than before.
Does levothyroxine cause weight loss?
It can help you lose the extra weight gained from hypothyroidism-usually 5-10 kg. But it’s not a weight-loss drug. If you’re already at a healthy weight, taking more than your prescribed dose won’t help you lose more. It just risks heart problems, bone loss, or anxiety. The goal is to restore normal metabolism, not speed it up.
Can I take levothyroxine with my other medications?
Some can interfere. Calcium, iron, antacids, and certain cholesterol drugs reduce absorption. Take them at least 4 hours apart. Also, avoid soy products and high-fiber meals within an hour of your dose. If you’re on multiple medications, ask your pharmacist to check for interactions. It’s easy to miss one.
Why do some people need higher doses than others?
Body weight is the biggest factor-larger people need more. But age, metabolism, other health conditions, and even genetics play a role. Women on estrogen therapy need higher doses. People with kidney or liver disease may process it slower. That’s why one-size-fits-all dosing doesn’t work. Your dose is personal, not generic.
Is there a natural alternative to levothyroxine?
Desiccated thyroid extract (like Armour Thyroid) comes from pig thyroids and contains both T4 and T3. Some patients prefer it, but studies show it’s less predictable and harder to dose accurately. The American Thyroid Association doesn’t recommend it as first-line treatment. It’s not “more natural”-it’s just a different hormone mix with less control. Stick with levothyroxine unless your doctor has a specific reason to switch.
If you’ve been told your thyroid is underactive, know this: you’re not broken. You’re not lazy. You just need the right hormone replacement-and the right routine to make it work. With levothyroxine, consistent dosing, and regular monitoring, most people get their energy, mood, and health back. It’s not magic. It’s medicine. And it works.

Katie Taylor
December 23, 2025 AT 16:29Finally, someone wrote this right. I was diagnosed with Hashimoto’s at 28 and thought I was just lazy. Levothyroxine didn’t fix me overnight, but after 6 months of consistency? I went from crying in the shower to running 5Ks. Stop blaming yourself-this is biology, not laziness.
Also, if your doctor won’t check ferritin or B12, find a new one. Iron deficiency is the silent saboteur here.
And yes, you can take it at night if mornings suck. I’m a nurse and I do it at 10pm after dinner. As long as it’s empty stomach, you’re golden.
Payson Mattes
December 25, 2025 AT 14:46Wait… so you’re telling me Big Pharma doesn’t want us to know that levothyroxine is just a Band-Aid? The real cause is glyphosate in our food supply and fluoride in the water-both destroy your thyroid. I’ve been taking kelp supplements and drinking apple cider vinegar in hot water since 2020, and my TSH dropped from 8.2 to 1.9 without meds. Your doctor won’t tell you this because they get kickbacks from Big Synthroid.
Also, soy milk is a poison. Don’t even get me started on how the FDA is complicit.
Adarsh Dubey
December 25, 2025 AT 15:04Excellent breakdown. I’ve been on levothyroxine for 12 years and still find myself rereading this. One thing I’d add: humidity degrading the pill is rarely discussed. I keep mine in a sealed glass jar with silica gel packs in the medicine cabinet. No more erratic TSH spikes.
Also, the 1.6 mcg/kg rule is a starting point, not gospel. My weight hasn’t changed in 5 years, but my dose went up 12.5 mcg last year because I started intermittent fasting. Your metabolism adapts. Monitor, don’t assume.
Jeffrey Frye
December 27, 2025 AT 03:48so like… i took my pill with coffee once bc i was late and then my tsh jumped to 12.5 and my doc was like ‘wtf’ and i was like ‘i thought it was just caffeine’ lol. also i switched brands last year and suddenly i felt like a zombie. turned out the filler in the generic had corn starch instead of lactose and my gut went haywire. so yeah, consistency matters. also, why do they make the pills so tiny? i lose half of them in the sink.
Andrea Di Candia
December 28, 2025 AT 23:36There’s a quiet dignity in managing this condition. It’s not glamorous. No one throws you a party when your TSH hits 2.1. But you show up. You take the pill. You get the blood test. You don’t give up because you’re tired. That’s not weakness-that’s resilience.
And if you’re still struggling even after all the labs look ‘normal’? You’re not broken. Your body is just asking for more patience, more nutrients, more listening. You’re not failing the treatment. The treatment is just learning you.
Be gentle with yourself. You’re doing better than you think.
Dan Gaytan
December 30, 2025 AT 01:39THIS. 🙌 I was on 100mcg for 2 years and still felt like a zombie. My doc said ‘your labs are fine’ but I knew something was off. Asked for ferritin-my iron stores were at 8. Normal is 15-150. After 3 months of iron, my energy came back like I’d been plugged in. Don’t settle for ‘normal’ labs if you don’t feel normal. You deserve to feel alive.
Also, levothyroxine at night works. I take mine at 9pm with water. No food. No phone scrolling. Just me, my pill, and peace. 🌙
Usha Sundar
December 30, 2025 AT 20:55I stopped taking it for 3 weeks. Felt like a ghost. Started again. Back to human. That’s it.
claire davies
December 31, 2025 AT 09:39As someone who moved from London to Melbourne and had to relearn the entire thyroid care system, I can tell you-this is the most comprehensive, humane, and accurate guide I’ve ever read. The bit about storage? Genius. I kept mine in the bathroom and wondered why my dose felt ‘off’. Turns out, humidity was eating my pills like a tiny, invisible raccoon.
Also, the fact that you mentioned the 25-50% increase in pregnancy? Vital. I was told ‘just take your usual dose’ when pregnant and ended up in the hospital with a TSH of 7.5. My baby’s neurodevelopment was fine, but I nearly didn’t make it through the first trimester. Please, if you’re expecting-get checked early, get checked often.
And yes, the cost difference between Synthroid and generic is insane. I paid $90/month in the US. Came back to the UK and got it free. It’s not about the medicine-it’s about the system. But the medicine? Still magic.
Chris Buchanan
December 31, 2025 AT 21:31Oh wow, so you mean to tell me that if I don’t take my pill before coffee, I’m basically just wasting $4 a month? And that I’ve been sabotaging myself for 4 years because I thought ‘it’s just one cup’? 🤦♂️
Also, ‘my doctor won’t check ferritin’? Bro, your doctor is probably just as tired as you are. Try saying ‘I need my iron levels checked because I’m still exhausted’ instead of ‘I think Big Pharma is lying’. It works better.
And yes, you can take it at night. I do. And I still have a life. Shocking, I know.
Raja P
January 2, 2026 AT 13:10Good post. I’ve been on levothyroxine for 8 years. One thing I learned: don’t compare your dose to others. My friend takes 75mcg, I take 150. We’re both fine. Body is weird. Trust your labs, not your Instagram thyroid group.
Joseph Manuel
January 4, 2026 AT 05:38The assertion that levothyroxine is the gold standard is empirically valid, though the article's reliance on survey data from the Thyroid Patient Advocate Foundation introduces selection bias. The sample is self-selected and non-randomized, rendering the 85% and 90% figures statistically non-generalizable. Additionally, the claim that ‘untreated hypothyroidism reduces life expectancy by 5–10 years’ lacks citation from longitudinal cohort studies. While the pharmacokinetics of levothyroxine are well-documented, the advice regarding nighttime dosing lacks peer-reviewed validation in major endocrine guidelines. Proceed with caution.
Harsh Khandelwal
January 6, 2026 AT 01:12lol so they want you to take a synthetic hormone for life but the real cure is ‘eat less soy’ and ‘take vitamin d’? sounds like a pyramid scheme. also why is this stuff so cheap? because it’s not supposed to cure you. it’s supposed to keep you hooked. next thing you know they’ll charge you $200 for a ‘thyroid energy boost’ app. i’m not taking it. i’m just gonna eat seaweed and pray.
Andy Grace
January 6, 2026 AT 16:31I’ve been on levothyroxine for 15 years. I used to think I was broken. Now I know I’m just tuned differently. The pill doesn’t change who I am-it just lets me be me again. No drama. No hype. Just consistency. And that’s enough.
Katie Taylor
January 7, 2026 AT 09:13Just read Joseph’s comment. Dude, I get you care about stats-but I’m not a study. I’m a person who cried in the parking lot before her first blood test. My TSH was 14. I took the pill. I ate the food. I slept. And now I’m here. You can’t measure hope in p-values.
Also, if you think ‘selection bias’ matters when someone’s life is on the line, maybe you need to stop reading medical journals and start listening to patients.