When you switch to a generic drug, you expect the same results as the brand-name version. But what if your body just doesn’t respond the same way - not because of quality, but because of your genes? For many people, the difference between a drug working perfectly or causing serious side effects comes down to inherited traits passed down through families. This isn’t theory. It’s happening right now in clinics, pharmacies, and homes across the UK and beyond.
Why Your Genes Matter More Than You Think
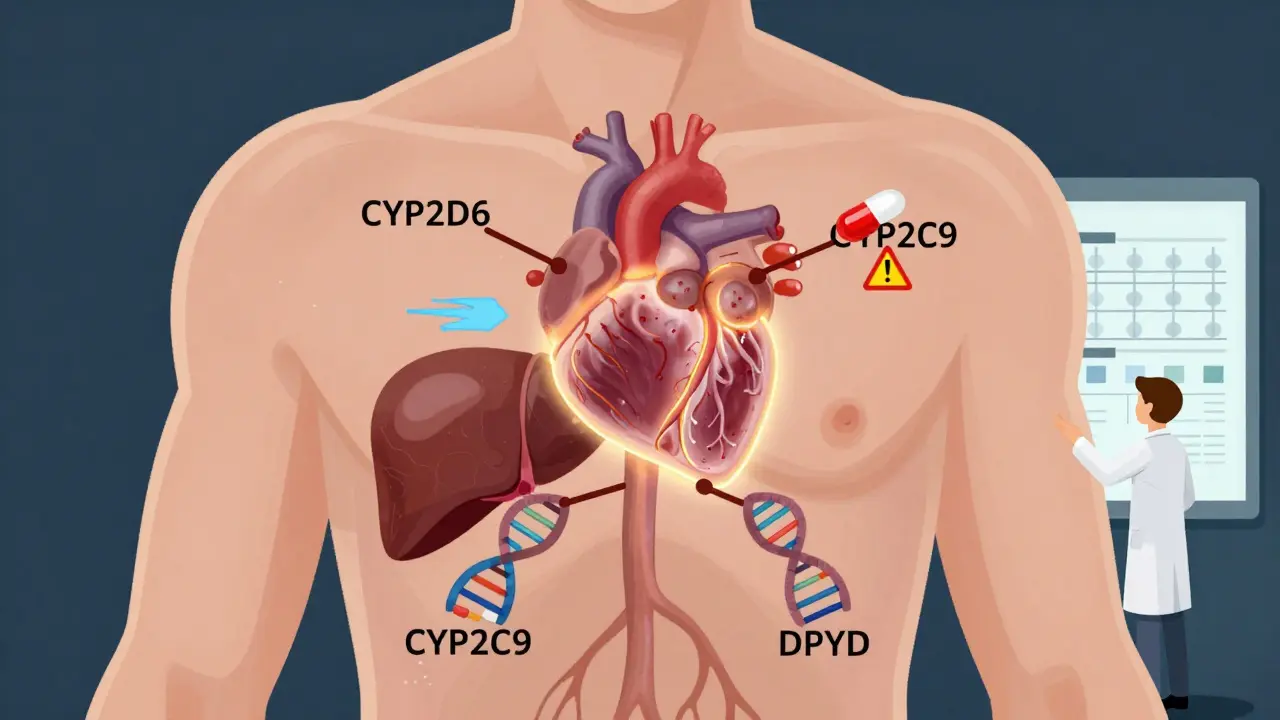
Generic drugs are chemically identical to their brand-name counterparts. That’s the law. But your body doesn’t see them that way. What matters is how your liver breaks them down - and that’s controlled by your DNA. The CYP2D6 gene alone affects how your body processes about 25% of all prescription drugs, including common antidepressants like sertraline, painkillers like codeine, and beta-blockers used for heart conditions. If you inherit two copies of a slow-metabolizer variant, your body can’t break down these drugs fast enough. The result? Toxic buildup. You might feel dizzy, nauseous, or even have a dangerous spike in heart rate. On the flip side, if you’re a rapid metabolizer, the drug leaves your system too quickly. You might think it’s not working - but it’s not the drug. It’s your genes. This isn’t rare. Around 7% of people in the UK are poor metabolizers of CYP2D6. That’s roughly 450,000 people who could be getting the wrong dose - or the wrong drug - without anyone knowing why.Family History Isn’t Just About Disease - It’s About Drugs
Think about your family. Did your mother have a bad reaction to a common painkiller? Did your uncle need a different antidepressant after three tries? These aren’t coincidences. They’re clues. Pharmacogenetics - the study of how genes affect drug response - shows that these patterns run in families. If your parent had severe side effects from a generic statin, you might too. If your sibling had to stop a blood thinner because of bleeding, your risk is higher. These aren’t just anecdotes. Studies show that up to 95% of variability in how people respond to certain drugs can be traced to inherited genetic differences. Take warfarin, a blood thinner often switched to generics. Two genes - CYP2C9 and VKORC1 - determine how much you need. Someone with certain variants might need half the dose of someone else. If your family has a history of bleeding on warfarin, you’re not just unlucky. You’re genetically at risk.Real Stories: When Genetics Saved - or Almost Broke - Someone
One patient in Manchester, a 58-year-old woman, was switched to a generic version of paroxetine after her insurance denied the brand. Within weeks, she developed severe dizziness and confusion. Her pharmacist noticed she’d been on the same dose for years - but her body had changed. A genetic test revealed she was a CYP2D6 poor metabolizer. Her dose was cut by 60%. Within days, she felt normal again. Another case was less lucky. A man in Leeds was prescribed a generic form of 5-fluorouracil for colon cancer. He developed life-threatening mouth sores and diarrhea. His family had no history of cancer - but his grandmother had died from chemo side effects decades ago. Genetic testing later showed he carried a rare DPYD variant that stops his body from breaking down the drug. He survived - but only because his oncologist had access to a pharmacogenomics database. Many aren’t so lucky.
Population Differences: Why One Size Doesn’t Fit All
Your ancestry matters. A 2024 study comparing Tunisian, Italian, and African populations found clear genetic differences in how people process common drugs. For example, the CYP2C19 gene variant that makes proton pump inhibitors (like omeprazole) less effective is found in 15-20% of Asians - but only 2-5% of Europeans. That means a generic proton pump inhibitor that works perfectly for someone of European descent might barely work for someone with South Asian ancestry. And it’s not just ancestry - it’s family lineage. If your grandparents came from a region with high rates of certain variants, you likely carry them too. Even warfarin dosing varies. African descent populations often need higher doses than Europeans because of differences in VKORC1 and CYP2C9. But most dosing guidelines still use average numbers - not genetic profiles. That’s why people from certain backgrounds are more likely to have dangerous bleeding or clots on generic blood thinners.What You Can Do - Before You Switch
You don’t need to wait for a crisis. Here’s what you can do today:- Ask your doctor: "Have you ever seen someone in my family have a bad reaction to a drug?" Write down the names and reactions.
- If you’ve had unexplained side effects from any medication - even over-the-counter ones - mention it. A rash, nausea, or dizziness could be genetic.
- Request a pharmacogenetic test if you’re starting a new drug, especially antidepressants, blood thinners, or chemotherapy. Tests like the Color Genomics panel or OneOme check 15+ genes for under £250.
- Ask if your GP or hospital uses the Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines. These are the gold standard for turning genetic results into dosing advice.
The Gap Between Science and Practice
Here’s the hard truth: most GPs don’t order these tests. Why? Time. Training. Lack of EHR integration. A 2023 survey of UK primary care doctors found that 79% wanted pharmacogenetic tools built into their electronic records - but only 12% had them. Most still rely on trial and error. That’s why patients keep getting the wrong dose. A 2022 Mayo Clinic study of 10,000 people who got preemptive testing found 42% had high-risk gene-drug matches. Of those, 67% had their meds changed - and adverse events dropped by 34%. The NHS is starting to move. In 2023, the UK’s Genomics England included pharmacogenetics in its 100,000 Genomes Project. But routine testing? Still not standard.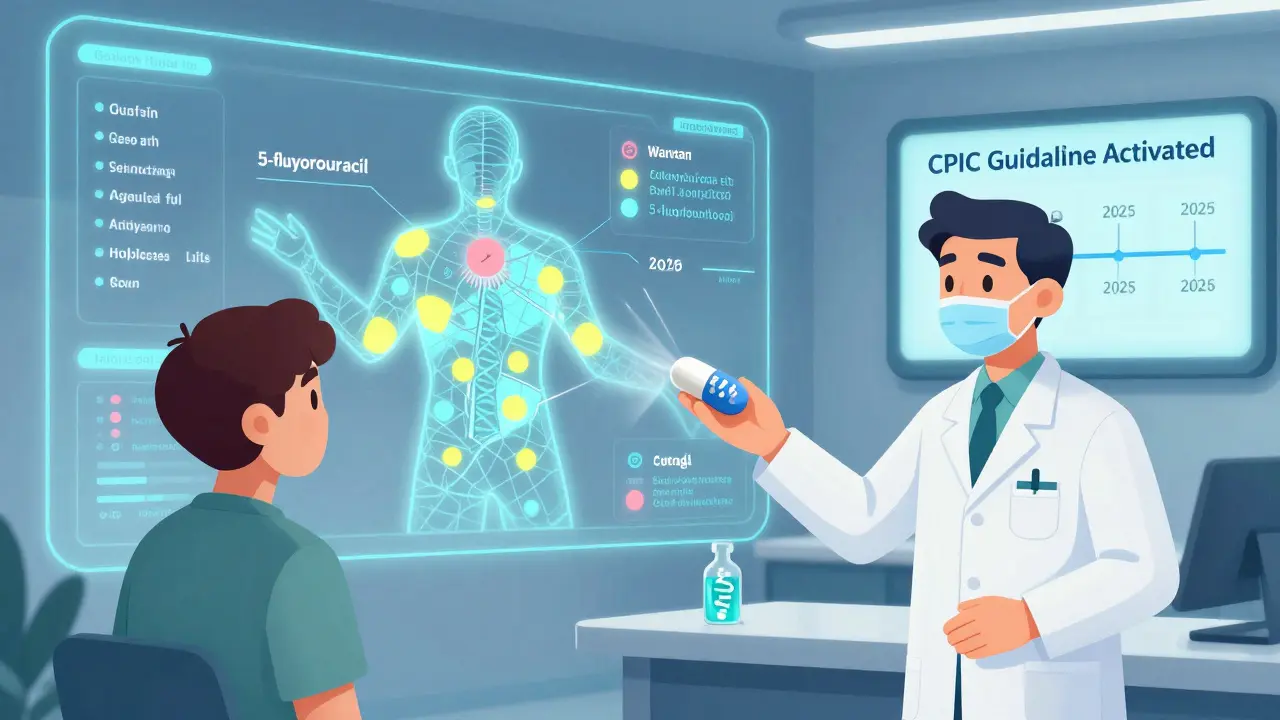
The Future: Personalized Generics
The next wave isn’t just about testing. It’s about using genetic data to design better generics. Imagine a version of paroxetine formulated for slow metabolizers - with slower release. Or a warfarin tablet that adjusts based on your CYP2C9 profile. That’s not sci-fi. It’s already in development. Companies like Genomind and OneOme are partnering with NHS trusts to embed genetic data into prescribing systems. By 2025, more than 90% of UK academic hospitals plan to offer preemptive testing. Community pharmacies? Slower. But change is coming.What to Ask Your Pharmacist
When you pick up a generic prescription, ask:- "Is this drug known to have genetic interactions?"
- "Have you seen patients with my background have issues with this?"
- "Can you check if my previous reactions match any known genetic risks?"
Bottom Line: Your Genes Are Your Prescription
Switching to a generic drug isn’t just about cost. It’s about your body’s unique biology. If your family has a history of drug reactions - or if you’ve had unexplained side effects - your genes may be the missing piece. Don’t wait for a bad reaction. Talk to your doctor. Ask for testing. Share your family history. You might just avoid a hospital stay - or worse.Genetics isn’t destiny. But ignoring it? That’s a risk you can’t afford to take.
Can family history really predict how I’ll react to a generic drug?
Yes. If close relatives had serious side effects from medications like blood thinners, antidepressants, or chemotherapy drugs, you may carry the same genetic variants. Studies show that up to 95% of variability in drug response is genetic, and these traits are often inherited. A family history of adverse reactions is one of the strongest indicators you may need genetic testing before starting a new drug.
Which genes are most important for generic drug response?
The most critical genes are CYP2D6 (metabolizes 25% of drugs), CYP2C9 and VKORC1 (affect warfarin dosing), CYP2C19 (impacts antidepressants and acid reducers), TPMT (controls thiopurine toxicity), and DPYD (breaks down 5-fluorouracil). These genes have well-documented links to serious side effects or treatment failure when variants are present.
Are generic drugs less safe because of genetic differences?
No. Generic drugs are chemically identical to brand-name versions. The issue isn’t quality - it’s how your body processes them. A person with a slow-metabolizer gene variant might have a dangerous reaction to a generic version of a drug they tolerated on the brand name - because the dose wasn’t adjusted for their genetics. The drug is fine. The dosing isn’t.
How accurate are pharmacogenetic tests?
For the major genes like CYP2D6, CYP2C9, and TPMT, tests are over 99% accurate in identifying variants. The challenge isn’t accuracy - it’s interpretation. Not all labs or doctors know how to translate results into dosing changes. That’s why using guidelines from CPIC or PharmGKB is critical.
Is pharmacogenetic testing covered by the NHS?
Currently, the NHS doesn’t routinely cover pharmacogenetic testing. But it may be offered in specific cases - like before starting chemotherapy or blood thinners - especially in academic hospitals. Private tests cost £200-£500. Some GP practices are beginning to offer them as part of personalized care programs, particularly for patients with complex drug histories.
Can I get tested before I even start a generic drug?
Yes. Preemptive testing - where you get tested before any drug is prescribed - is becoming more common. Hospitals like Mayo Clinic and Vanderbilt have shown that testing patients upfront can prevent 30-40% of adverse drug events. In the UK, initiatives like Genomics England are paving the way. Talk to your GP about whether preemptive testing is available in your area.

Susan Kwan
February 8, 2026 AT 16:46Okay but let’s be real - if your doctor doesn’t even know what CYP2D6 stands for, why are we pretending this isn’t just a $$$ game? I’ve had my meds switched to generics three times. Each time, I felt like a zombie. No one asked about my family history. My mom died on a generic blood thinner. Guess what? They didn’t test me. They just said ‘it’s the same drug.’
Same drug? My body says otherwise.
MANI V
February 8, 2026 AT 17:04Typical Western nonsense. In India, we don’t need fancy gene tests. We’ve been using generics for decades. If you get sick, you’re weak. Your body should adapt. Why are you so fragile? Your genes? Pfft. My uncle took warfarin for 20 years without a single test. He’s fine. You just need discipline.
Stop blaming your DNA. Start blaming your laziness.
Random Guy
February 9, 2026 AT 08:52so like… if my grandma had a bad reaction to aspirin in 1973, does that mean i’m genetically doomed to explode if i take ibuprofen? 🤔
also why does every article about this sound like a sci-fi trailer? ‘THE DRUGS… THEY KNOW YOUR DNA…’
my pharmacist just handed me a pill and said ‘here ya go’
so… i’m just supposed to google my ancestry and hope for the best? 🤷♂️
Ryan Vargas
February 9, 2026 AT 23:57Let’s not pretend this is merely about pharmacogenetics. This is a systemic dismantling of individual biological sovereignty under the guise of cost-cutting. The pharmaceutical-industrial complex doesn’t want you to know that your genetic uniqueness is a liability - because personalized dosing doesn’t scale. Generics are the new standardization: one-size-fits-none, but they’ll make you believe it’s one-size-fits-all.
And don’t get me started on how the NHS, despite its rhetoric, has no infrastructure to support preemptive testing - because if they did, they’d have to admit that their entire drug approval model is based on population averages that are statistically irrelevant to your unique genome.
This isn’t medicine. It’s demographic engineering. And the fact that 79% of GPs want tools they don’t have? That’s not negligence. That’s intentional obfuscation.
They’re not ignoring your genes. They’re erasing them.
Tasha Lake
February 11, 2026 AT 04:13As someone who works in clinical pharmacology, I’ve seen this firsthand. The CYP2D6 poor metabolizer phenotype is way more common than people think - especially in South Asian populations where the *CYP2D6*4 allele is prevalent. But here’s the kicker: most generic formulations aren’t bioequivalent in terms of pharmacokinetics, even if they’re chemically identical. The excipients? The dissolution profiles? They vary.
So you’ve got a genetic predisposition PLUS formulation variability = perfect storm. We’re not just talking about dosing - we’re talking about bioavailability differences that aren’t captured in current regulatory standards.
CPIC guidelines are gold standard, but they’re useless if your EMR doesn’t auto-flag high-risk combinations. We need integrated genomic decision support - not after the fact, but pre-prescription.
Sam Dickison
February 11, 2026 AT 20:40My sister’s on a generic antidepressant. She went from chill to crying in the grocery store. No one asked about her dad’s history with Zoloft. Turns out - he had the same reaction. We got her tested. CYP2D6 ultra-rapid metabolizer. She needed 3x the dose. They gave her half. She almost quit her job.
Why does this feel like a lottery? We test dogs for breed traits. We test babies for Down syndrome. But your body’s reaction to medication? Nah. Wait till you’re hospitalized.
Just… ask. Always ask.
Brett Pouser
February 13, 2026 AT 13:59As a first-gen American with roots in rural Bangladesh, this hits different.
My aunt had a stroke on warfarin. They said ‘it’s just how it is.’ But her cousin had the same drug and was fine. Turns out - both had the same VKORC1 variant. My whole side of the family? High risk. No one told us.
I got tested last year. CYP2C19 poor metabolizer. That’s why omeprazole never worked for me. I thought I was just ‘sensitive.’ Turns out - I was genetically coded to need a different drug.
Family history isn’t gossip. It’s your medical blueprint. Stop waiting for permission to ask. Go get tested.
Simon Critchley
February 14, 2026 AT 03:58Right. So let me get this straight - we’re saying that a £250 spit test could’ve saved me from 3 hospital trips? 😂
My GP laughed when I asked. Said ‘you’re not a cancer patient.’
Meanwhile, my mate got his genes tested because he wanted to know if he’s got ‘Nordic warrior DNA.’ Turns out he’s a CYP2D6 poor metabolizer. He’s been on paroxetine for 8 years. No wonder he felt like a zombie.
It’s not science. It’s a conspiracy of silence. And we’re all just waiting for someone to die before they listen.
PS: I got my results. My pharmacist printed them out. She said ‘this is why I love my job.’ 😭
Karianne Jackson
February 14, 2026 AT 17:25I took a generic painkiller and passed out. My mom did the same thing. We didn’t know why. Now I know. My genes. I’m so mad.
Tom Forwood
February 15, 2026 AT 11:06yo i just got my color genomics report back and holy crap - i’m a CYP2C19 poor metabolizer AND a CYP2D6 ultra-rapid. that means my antidepressant? it’s basically useless. and my pain meds? they’re poisoning me.
my doc didn’t even know what the report meant. i had to show him the pharmgkb page.
but here’s the good part - i switched to a brand-name drug with adjusted dosing. i haven’t felt this good in years.
if you’ve ever been like ‘wtf is wrong with me?’ - get tested. it’s not expensive. it’s not scary. it’s just… information.
your body’s been screaming. finally, someone listened.