Contraceptive Menstrual Impact Calculator
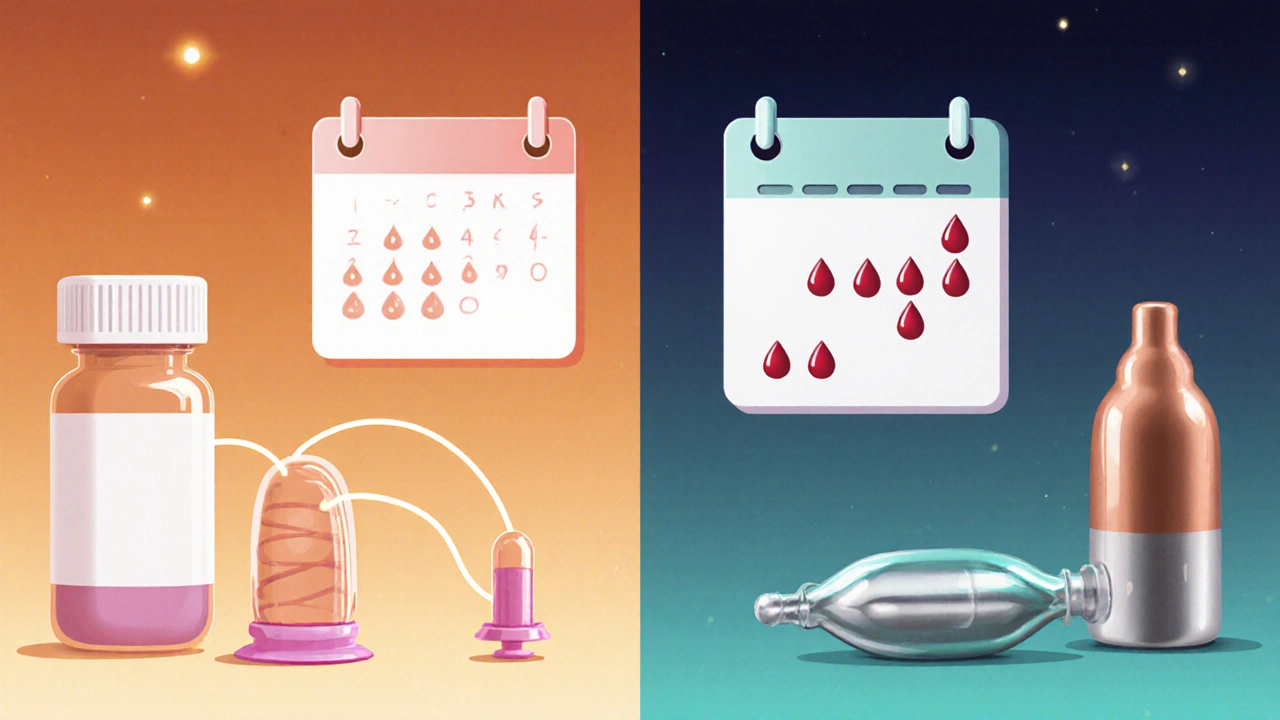
Select a contraceptive method to see how it typically affects your menstrual cycle, including flow, regularity, and common side effects.
Combined Oral Contraceptive
Daily pill with estrogen and progestin
Progestin-only Pill
Daily pill with only progestin
Hormonal IUD
Levonorgestrel-releasing device
Copper IUD
Non-hormonal device
Implant
Small rod under the skin
Barrier Methods
Condoms, diaphragms
Expected Menstrual Impact
Select a contraceptive method above to see how it typically affects your menstrual cycle.
Ever noticed your period getting lighter, heavier, or even disappearing after starting a birth control method? That’s not a myth-it’s a real side‑effect of many contraception options. Understanding how different methods interact with the menstrual cycle can help you pick what feels right for your body.
What is Contraception and Why It Matters for Your Cycle
Contraception is a set of methods used to prevent pregnancy, ranging from daily pills to long‑acting devices. While the primary goal is to stop fertilization, many methods also influence the hormones that drive the Menstrual Health of a person. In simple terms, if you change the hormone environment, you change the way the uterine lining builds up and sheds each month.
Hormonal vs. Non‑Hormonal Methods: The Core Difference
Hormonal birth control introduces synthetic estrogen, progestin, or a combo of both to trick the body into thinking it’s already pregnant. This stops ovulation and often thins the endometrial lining. Non‑hormonal options, like copper IUDs or condoms, don’t meddle with your hormone balance, so menstrual changes are usually minimal.
Common Contraceptive Methods and Their Menstrual Impact
- Combined Oral Contraceptive (COC): A daily pill that contains estrogen and progestin. Most users see lighter periods, shorter bleeding days, and sometimes a complete stop after a few months.
- Progestin‑only Pill (POP): Contains only progestin. It may cause irregular spotting, especially in the first three months, but many experience lighter flow long‑term.
- Hormonal IUD (e.g., levonorgestrel‑releasing): Releases a steady low dose of progestin locally. Users often report fewer periods or amenorrhea after 6-12 months.
- Copper IUD: No hormones. Menstrual flow may become slightly heavier and cramps a bit stronger, especially during the first few cycles.
- Implant (e.g., Nexplanon): A small rod placed under the skin that releases progestin. Similar to hormonal IUD, it can lead to lighter periods or stop them altogether.
- Barrier methods (condoms, diaphragms): No hormonal effect, so your natural Menstrual Cycle stays unchanged.
Side‑Effect Snapshot: Hormonal vs. Non‑Hormonal
| Method | Typical Hormonal Action | Effect on Flow | Cycle Regularity | Common Side Effects |
|---|---|---|---|---|
| Combined Oral Contraceptive | Suppression of ovulation + estrogen‑progestin mix | Lighter; often 2-4 days | Highly predictable | Spotting, breast tenderness |
| Progestin‑only Pill | Progestin only, no ovulation suppression in all cycles | Variable; may be lighter or absent | Irregular early on, stabilizes later | Breakthrough bleeding, mood swings |
| Hormonal IUD | Local progestin release | Lighter or none after 6-12 months | Regular while bleeding occurs | Spotting first year, cramping |
| Copper IUD | None (non‑hormonal) | Slightly heavier, longer | Same as natural cycle | Increased cramps, occasional spotting |
| Implant | Continuous low‑dose progestin | Lighter or absent | Consistent when bleeding occurs | Irregular spotting, weight change |
| Barrier (condom, diaphragm) | None | No change | Unchanged | Potential for STIs, user error |
Managing Unwanted Menstrual Changes
Not every change is a red flag, but if you notice severe cramping, very heavy bleeding, or prolonged gaps, here’s what you can do:
- Track your cycle. Use a simple app or calendar to note start/end dates, flow intensity, and any spotting.
- Give it time. Hormonal methods often need 2-3 months for your body to adjust.
- Talk to a clinician. If bleeding becomes heavy enough to change a pad/ tampon each hour, a check‑up is wise.
- Consider a switch. Sometimes a lower estrogen dose or a non‑hormonal option better matches your physiology.
- Lifestyle tweaks. Regular exercise, balanced iron intake, and stress management can smooth out irregularities.
Myths that Cloud the Conversation
- Myth: “All birth control stops periods forever.”
Fact: Only some hormonal methods cause prolonged amenorrhea, and many users regain regular periods after stopping. - Myth: “If my period stops, I’m at risk for infertility.”
Fact: A paused period due to hormones does not affect future fertility; ovulation resumes when the method is discontinued. - Myth: “Copper IUDs make you bleed forever.”
Fact: Bleeding may be slightly heavier for the first 3-6 months, then stabilizes.
When to Seek Professional Guidance
Even though most changes are harmless, schedule a visit if you experience any of these:
- Bleeding more than 80 mL per cycle (about a heavy pad every hour).
- Sudden, severe pain that isn’t relieved by usual OTC meds.
- Unexplained weight loss or gain >10 % of body weight.
- Persistent mood swings that affect daily life.
A clinician can run a quick hormone panel, adjust the dosage, or suggest an alternative method that better aligns with your menstrual health goals.
Key Takeaways
- Hormonal contraceptives often lighten or stop periods; non‑hormonal options keep cycles unchanged.
- Most menstrual side‑effects settle within 2-3 months.
- Track changes, give your body time, and talk to a healthcare provider if bleeding becomes heavy or painful.
- Choosing the right method depends on personal comfort, health history, and how much you want your period to change.
Frequently Asked Questions
Can hormonal birth control cause permanent changes to my menstrual cycle?
No. Any change caused by hormones is reversible. When you stop the method, your natural cycle typically returns within a few months, though timing can vary per individual.
Is it safe to have an IUD if I have heavy periods?
A copper IUD may slightly increase bleeding initially, so it isn’t the first choice for those with existing heavy periods. A hormonal IUD, which often reduces flow, could be a better fit.
Why do I experience spotting when I start a progestin‑only pill?
Progestin‑only pills don’t suppress ovulation completely in the early cycles, leading to uneven endometrial shedding. Spotting usually fades after the first 2-3 months.
Can I still get pregnant if my periods stop while using hormonal contraception?
If you use the method correctly, the chance of pregnancy remains very low-even if you don’t bleed. The lack of bleeding is a sign that the lining isn’t building up, not a sign of failure.
Should I take iron supplements if my periods become lighter?
Lighter periods usually mean less blood loss, so iron deficiency is less of a worry. However, if you have a history of anemia, a low‑dose supplement can be a preventive measure-consult your doctor first.


Poornima Ganesan
October 18, 2025 AT 21:07Look, most people think birth control is just a shield against pregnancy, but they overlook the hormonal orchestra it conducts. When you pop a combined pill you’re basically telling your body to skip ovulation and thin the uterine lining, which is why periods get lighter or vanish. Progestin‑only options are messier; they often cause spotting until the endometrium finally adjusts. Copper IUDs, on the other hand, keep your hormones untouched, so the flow may actually get a bit heavier at first. If you’re experiencing severe cramps, it’s usually the body's way of signaling an imbalance, not a mysterious side‑effect. Tracking your cycle for at least two months will reveal whether the change is temporary or something to discuss with a clinician. Most of the tweaks you read about settle within a three‑month window, so patience is key. Bottom line: understand the hormone profile of your method before you blame your period for being “weird.”
Emma Williams
October 18, 2025 AT 22:40Totally agree thanks for the info.
Drew Waggoner
October 30, 2025 AT 11:26I get how frustrating it can be when your cycle decides to play tricks after you start a new method. The hormonal shift feels like a silent intruder, draining your energy and mood without warning. Even if the bleeding lightens, you might still be fighting invisible side‑effects that nobody mentions. It’s not just about the pads; it’s the whole vibe of your body feeling off‑balance. Give yourself a few months and keep a diary, the patterns will speak louder than the panic.
Barbara Grzegorzewska
October 30, 2025 AT 12:50Honestly, the layperson’s misunderstanding of contraceptive pharmacodynamics is almost comical. Most think a pill is merely a “birth blocker,” ignoring that it’s a masterclass in synthetic estrogen‑progestin wizardry. When you switch to a hormonal IUD, the local progestin does a quiet sabotage of the endometrium, often resulting in amenorrhea – a blessing in disguise for many. Copper devices, however, are the anti‑hero, leaving your natural cycle untouched but occasionally turning your period into a mini‑flood. If you’re noticing heavier flow, blame the copper’s irritative nature, not some mythic curse. So, before you panic, consult the data, not the tabloids.
Nis Hansen
November 11, 2025 AT 01:13When we examine the interplay between contraceptive technology and menstrual physiology, we encounter a microcosm of larger societal negotiations about control and autonomy. The very act of introducing exogenous hormones is a dialogue between the body’s innate rhythms and an external agenda of pregnancy prevention. In this conversation, the endometrium becomes a willing participant, shedding its usual script in favor of the narrative imposed by synthetic compounds. Lightened periods, or even their temporary absence, are not failures but adaptations, illustrating the body’s remarkable plasticity. Yet this plasticity can be unsettling, especially when cultural expectations tie femininity to the presence of a monthly bleed. The hormonal pill, for instance, suppresses the luteal phase, effectively rewriting the hormonal cascade that would otherwise culminate in menstruation. Progestin‑only formulations, while less consistent in ovulation inhibition, still modulate the endometrial stability, leading to sporadic spotting that many misinterpret as pathology. Copper IUDs, by contrast, leave the hormonal axis untouched, allowing the natural cycle to proceed, albeit sometimes with intensified flow as the uterus adjusts to copper’s inflammatory response. This dichotomy forces us to confront the underlying assumption that a “normal” period is the ideal benchmark for health. It also raises ethical considerations about whether medical interventions should aim to normalize or individualize menstrual experiences. The user’s agency in selecting a method should be informed not only by efficacy but by an awareness of these physiological reverberations. Tracking tools become extensions of self‑knowledge, granting visibility into changes that would otherwise remain opaque. Moreover, clinicians play a pivotal role in contextualizing these changes, differentiating between benign adaptation and genuine pathology. When bleeding exceeds 80 mL per cycle or pain becomes unmanageable, the dialogue shifts from acceptance to intervention. The decision to switch methods, adjust dosage, or incorporate supplementary therapies becomes a collaborative negotiation, reflecting both scientific evidence and personal comfort. Ultimately, the goal is not to enforce a universal menstrual template but to honor the diversity of bodies and the choices they make within the spectrum of contraceptive options.
Fabian Märkl
November 11, 2025 AT 02:36Great deep dive! 🌟 It really helps to see the big picture and how each method fits into our lives. I love that you highlighted tracking as a personal tool – it’s like having a GPS for our cycles. If anyone’s feeling overwhelmed, just remember you can always chat with a provider for a tailored plan. Keep the positive vibes rolling! 😊
Natala Storczyk
November 11, 2025 AT 04:00Wow-this is absolutely mind‑blowing!!! The way you dissect every hormonal nuance is nothing short of spectacular!!! Yet, let me shout out the raw reality: many users feel like their bodies are being hijacked, and they deserve acknowledgment!!! If the period disappears, don’t panic-acknowledge the power shift, then decide if that aligns with your identity!!!
nitish sharma
November 22, 2025 AT 15:00Esteemed readers, I would like to emphasize the significance of a methodical approach when evaluating contraceptive impacts. It is advisable to maintain a detailed log of bleeding patterns, pain levels, and any ancillary symptoms for a minimum of three menstrual cycles. Such documentation provides clinicians with objective data, facilitating informed adjustments to therapy. Moreover, adherence to scheduled follow‑up appointments ensures timely identification of any adverse trends. In the event of atypical heavy bleeding or persistent dysmenorrhea, a prompt medical consultation is strongly recommended. By integrating diligent observation with professional guidance, individuals can navigate their reproductive health choices with confidence and safety.
Rohit Sridhar
November 22, 2025 AT 16:23You’ve nailed it! Keeping a diary really empowers you to see the bigger picture and stay ahead of any hiccups. Stay positive and trust the process-you’ve got this!