GLP-1 Weight Loss Estimator
Estimate potential weight loss based on clinical trial data from FDA-approved GLP-1 medications. Note: Results vary based on individual factors and adherence.
Estimated Weight Loss
When you think of diabetes medications, you probably picture pills that lower blood sugar. But today, the most talked-about drugs in this class aren’t just for diabetes-they’re reshaping how we treat obesity. Drugs like Ozempic, Wegovy, and Mounjaro were originally designed to help people with type 2 diabetes manage their blood sugar. But something unexpected happened: patients started losing weight-sometimes a lot of it. And that’s turned these medications into one of the biggest medical breakthroughs of the decade.
How GLP-1 Agonists Actually Work
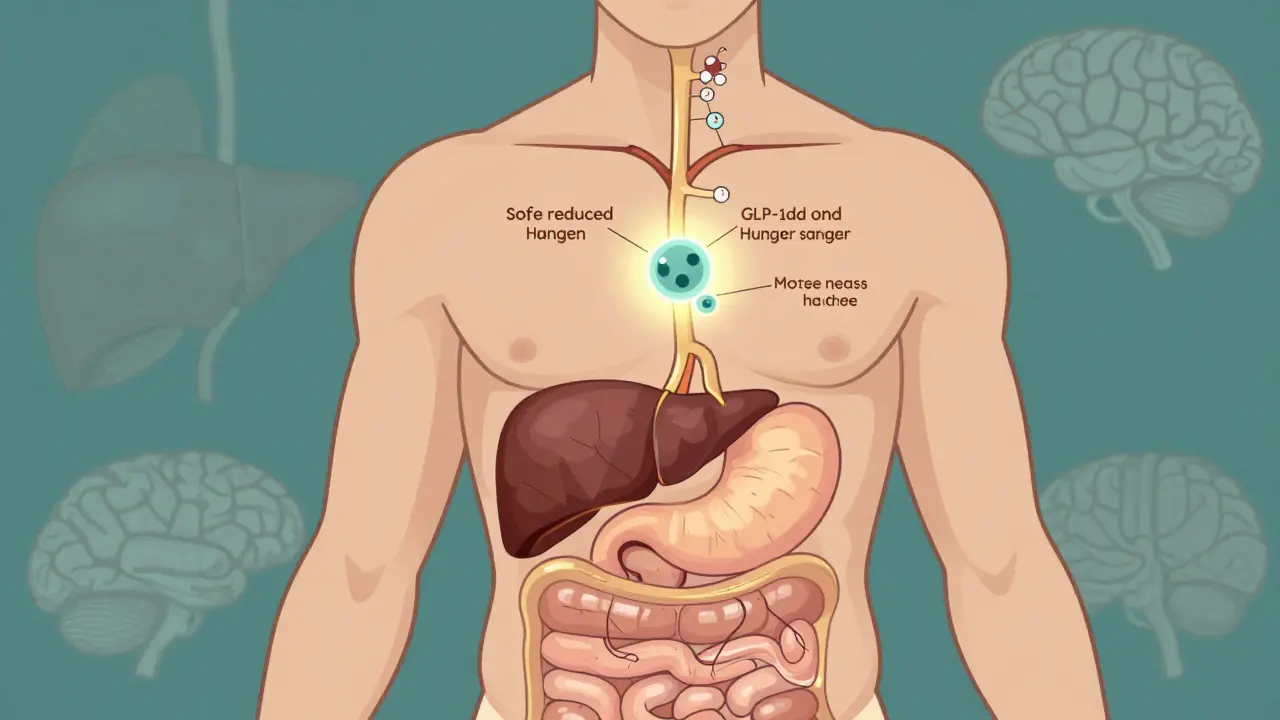
GLP-1 agonists mimic a hormone your body already makes called glucagon-like peptide-1. This hormone does three important things: it tells your pancreas to release insulin when your blood sugar rises, it stops your liver from dumping out too much glucose, and it slows down how fast food leaves your stomach. That last part is key for weight loss. When food moves slowly through your gut, you feel full longer. But the real game-changer is what happens in your brain. These drugs act on areas that control hunger and cravings, making you less interested in food-especially high-calorie, sugary stuff.
Unlike insulin or sulfonylureas, which often cause weight gain, GLP-1 agonists help you lose weight without making you hungrier. That’s why they’ve become the go-to option for people with type 2 diabetes who also struggle with obesity. But the benefits go even further. Studies show they lower blood pressure, improve cholesterol levels, and reduce inflammation-all factors that drive heart disease.
Weight Loss That Actually Sticks (For a While)
Let’s talk numbers. In clinical trials, people using semaglutide (Wegovy) at the full 2.4 mg weekly dose lost an average of 15% of their body weight over 68 weeks. That’s not a few pounds-it’s 30 to 50 pounds for many people. Tirzepatide (Mounjaro, Zepbound) did even better. In one study, nearly 60% of participants on the highest dose lost 20% or more of their body weight. For someone weighing 200 pounds, that’s 40 pounds gone.
Compare that to diet and exercise alone. In the STEP-1 trial, people who just changed their lifestyle lost about 2.4% of their weight. Those who added Wegovy lost nearly 15%. That’s a six-fold difference. And it’s not just about the scale. People report fewer cravings, less binge eating, and more control over food choices. One Reddit user described it as “my brain finally stopped screaming for snacks.”
But here’s the catch: these results only last as long as you keep taking the drug. When people stop, most regain 50 to 70% of the weight within a year. That’s not failure-it’s biology. Your body fights to return to its old weight, and without the drug, hunger signals come roaring back. That’s why experts say GLP-1 agonists aren’t a cure-they’re a tool. Like blood pressure meds, you may need them long-term.
Who Benefits the Most?
These drugs work best for people with obesity and type 2 diabetes, prediabetes, or existing heart disease. In fact, the American Diabetes Association now recommends GLP-1 agonists as a first-line treatment for type 2 diabetes patients who also have excess weight or cardiovascular issues. That’s a huge shift-from seeing them as a backup to seeing them as a front-line defense.
But they’re not magic for everyone. If you’re lean, have no metabolic issues, and just want to lose 10 pounds for aesthetic reasons, the risks may outweigh the benefits. The side effects-mainly nausea, vomiting, and diarrhea-can be tough. About half of users experience them early on, though most fade after a few weeks. People with a history of pancreatitis, gallbladder disease, or certain thyroid cancers are usually advised to avoid them.
And while they’re approved for weight loss in adults with a BMI over 30 (or over 27 with a weight-related condition), many doctors are prescribing them off-label for people just below that threshold. IQVIA found that in 2023, 60% of semaglutide prescriptions were for weight loss, not diabetes. That’s a sign of how powerful the demand is.
The Dark Side: Side Effects, Cost, and "Ozempic Face"
Let’s be real-these drugs aren’t easy. Nausea is the most common side effect. About 30% of users report it, and 10% say it’s bad enough to affect their daily life. Vomiting and diarrhea are also common, especially when starting or increasing the dose. That’s why doctors start low: 0.25 mg weekly for the first month, then slowly bump up over 4 to 5 months. Skipping steps can make side effects worse.
Then there’s the cost. Without insurance, Wegovy runs about $1,350 a month. Even with insurance, many people pay hundreds out of pocket. A 2024 survey found 58% of users struggled with coverage. Some people ration their doses-taking half to stretch their supply-putting their health at risk. Novo Nordisk offers a savings program that covers 75% of costs for eligible patients, but it doesn’t help everyone.
And then there’s "Ozempic face." It’s not a medical term, but it’s everywhere on social media. Long-term users report losing facial fat, looking gaunt, or appearing older than they are. Harvard Health reported this in 42% of long-term users. It’s not dangerous, but it’s startling. Dermatologists are seeing more patients asking for fillers to restore volume. This isn’t a reason to avoid the drug, but it’s something to know before you start.
Beyond Weight: Surprising Brain and Heart Benefits
Here’s where things get really interesting. GLP-1 agonists aren’t just helping people lose weight-they’re protecting their hearts. In a 2024 study by Dr. Eric Polley, users had 12-18% fewer heart attacks, strokes, and heart-related deaths. That’s why Ozempic and Victoza are FDA-approved to reduce cardiovascular events in people with diabetes and heart disease.
But the brain benefits? That’s the surprise. A 2024 study of 2 million U.S. veterans found GLP-1 users had 23% fewer seizures, 17% lower risk of substance addiction (including alcohol and opioids), and 14% less suicidal thinking. Researchers are now testing these drugs for Alzheimer’s, Parkinson’s, and even depression. Early results are promising. One theory: GLP-1 receptors are found throughout the brain, and activating them may reduce inflammation and protect nerve cells.
Even more unexpected: a 16% drop in eating disorders like bulimia, and an 11% lower risk of psychotic disorders like schizophrenia. These aren’t side effects-they’re therapeutic effects. We’re just starting to understand how wide-ranging these drugs can be.
What’s Next? The Future of GLP-1 Drugs
The market for these drugs is exploding. Global sales hit $35.7 billion in 2023 and could hit $100 billion by 2030. Why? Because the need is huge. Nearly half of U.S. adults have obesity. But only 2% of eligible people are on these drugs right now. The bottleneck? Cost and supply.
Next-gen versions are already in the works. Oral semaglutide at higher doses (50 mg) is in Phase 3 trials. There are also triple agonists that target GLP-1, GIP, and glucagon at once-potentially boosting weight loss even more. Implants that last 6 to 12 months are being tested, which could solve the injection and adherence problem.
Companies like Amazon and Walmart are adding GLP-1 drugs to employee health plans. Insurance companies are scrambling to figure out how to cover them without bankrupting their budgets. Meanwhile, doctors are learning how to use them better-pairing them with nutrition coaching, movement, and mental health support. Programs like Calibrate and Found offer all three, but cost $99 to $149 a month on top of the drug.
Final Thoughts: A Tool, Not a Miracle
GLP-1 agonists are powerful. They’ve changed the lives of millions who struggled with weight, diabetes, and heart disease. But they’re not a quick fix. They require commitment, medical supervision, and an understanding that weight loss is just one part of the story. The real win isn’t just the number on the scale-it’s better blood pressure, fewer heart problems, clearer thinking, and less craving.
They’re not for everyone. But for those who need them, they’re one of the most effective tools we’ve ever had. The challenge now isn’t just making them work-it’s making them accessible, sustainable, and safe for the long term.

Cam Jane
January 5, 2026 AT 11:43I’ve been on Wegovy for 10 months and honestly? My brain finally stopped screaming for snacks. I used to snack at 2am like it was my job. Now? I forget I’m hungry until lunch. The nausea sucked at first, but after week 3 it vanished. I lost 42 pounds and my blood pressure dropped like it owed me money. Not magic. Just biology working the way it should.
Also, Ozempic face? Real. I look like I lost a bet with a mirror. Got filler in my cheeks last month. Worth it.
Venkataramanan Viswanathan
January 5, 2026 AT 11:57These medications represent a paradigm shift in metabolic medicine, grounded in robust neuroendocrinological mechanisms. The GLP-1 receptor is ubiquitously expressed in the central nervous system, particularly in the hypothalamus and brainstem, where it modulates satiety signaling through POMC and NPY neurons. The clinical efficacy observed in trials is not merely anecdotal but statistically significant across multiple cohorts with p-values < 0.001. However, long-term safety data beyond five years remain limited, and cost-effectiveness analyses in low-income populations are critically underdeveloped.
Beth Templeton
January 6, 2026 AT 17:08So you’re telling me a drug that makes you puke and costs a mortgage payment is now the new diet? Cool. I’ll stick with eating less and moving more. Oh wait that’s not profitable enough.
Ryan Barr
January 8, 2026 AT 12:1215% weight loss? Cute. I lost 22% on a 30-day fast and didn’t need a $1300 injection. This is just pharma’s way of monetizing hunger.
Molly McLane
January 9, 2026 AT 08:31For anyone considering this: talk to your doctor, yes-but also talk to people who’ve been on it. The side effects aren’t just nausea. Some people get severe reflux, others feel emotionally numb. I lost weight but felt like I was watching my life through glass. It’s not a villain, but it’s not a hero either. It’s a tool. And tools can cut both ways.
If you’re doing this for looks? Pause. If you’re doing it because your health is at risk? That’s different. You deserve support, not judgment.
Wesley Pereira
January 11, 2026 AT 01:50Y’all act like Ozempic is some newfangled miracle but it’s just another corporate cash grab wrapped in biohype. Pharma’s been pushing ‘weight loss drugs’ since fen-phen. The real win? They’re finally making people care about metabolic health. But the access gap? Wild. I work in primary care. Half my patients ration doses. One guy split his 1mg pen into 4 doses to make it last. Dude’s not dumb-he’s desperate.
And the ‘Ozempic face’ thing? Yeah, it’s real. But so is the fact that 80% of these folks had zero access to nutritionists or therapy. We’re treating symptoms because we refuse to fix systems.
Isaac Jules
January 11, 2026 AT 07:24Stop glorifying this shit. You think losing weight with a drug makes you better than someone who diets? You’re just a walking billboard for Big Pharma. People on these drugs are literally buying their self-worth. And the ‘brain benefits’? That’s just correlation with a fancy name. You think reducing cravings means you’re smarter? Nah. You’re just chemically sedated.
And don’t get me started on the ‘Ozempic face’-you look like a zombie because you’re starving your body. Congrats. You traded your face for a number on a scale. Pathetic.
Dana Termini
January 11, 2026 AT 08:25I’ve been on Mounjaro for 8 months. Lost 56 lbs. My A1C dropped from 8.2 to 5.4. I sleep better. I don’t panic-eat when I’m stressed. But I also cry sometimes because I miss the way food used to comfort me. It’s not just about the weight. It’s about identity.
To the people saying this is lazy? I’ve been trying to lose weight since I was 16. I’ve done keto, intermittent fasting, Weight Watchers, juicing, cleanses, and 3 different personal trainers. Nothing worked. This did. Not because I’m weak. Because my body needed a different tool.
We need better access. Not shame.