Chronic eczema isn’t just dry skin. It’s a broken barrier, a misfired immune system, and an unrelenting itch that steals sleep, confidence, and days of your life. If you’ve been treating it like a simple rash-slathering on lotion when it flares and ignoring it the rest of the time-you’re not alone. But here’s the truth: chronic eczema starts long before the redness shows up. The real problem isn’t inflammation-it’s a leaky skin barrier. And fixing that is the single most effective thing you can do.
Why Your Skin Barrier Is the Root Cause
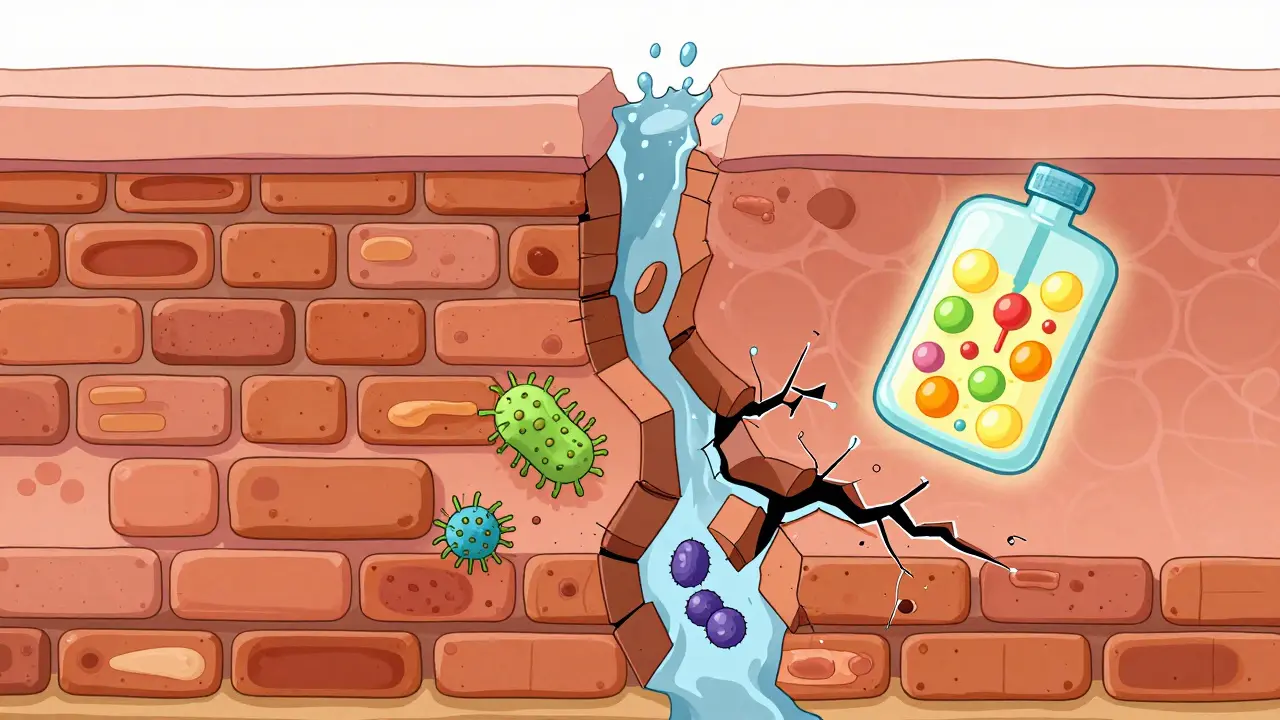
Your skin isn’t just a surface. It’s a layered fortress. The top layer, called the stratum corneum, is made of dead skin cells held together by lipids-fats like ceramides, cholesterol, and free fatty acids. Think of it like a brick wall where the bricks are skin cells and the mortar is these lipids. In chronic eczema, that mortar is crumbling. Studies show people with moderate to severe eczema have 30-50% less ceramide than healthy skin. That’s not a coincidence. It’s the reason water escapes, irritants get in, and bacteria like Staphylococcus aureus take over.This isn’t new science. Since 2006, researchers have known that mutations in the filaggrin gene (FLG) are present in about half of all severe eczema cases. Filaggrin breaks down into natural moisturizing factors that keep skin hydrated. When it’s missing, your skin dries out faster. People with this mutation often have TEWL (transepidermal water loss) readings of 25-40 g/m²/h. Healthy skin? 8-12 g/m²/h. That’s a 300% increase in moisture loss. No wonder your skin feels tight, cracked, and raw.
And here’s the kicker: barrier damage happens before the itch. In high-risk infants, studies show the skin barrier breaks down 3-6 months before the first visible flare. That’s why prevention starts before the rash appears. Repairing the barrier isn’t a treatment-it’s the foundation of every successful eczema plan.
What Actually Repairs the Barrier (And What Doesn’t)
Not all moisturizers are created equal. A basic petrolatum ointment or cheap lotion might feel soothing, but it doesn’t fix the problem. It just sits on top like plastic wrap. Real barrier repair means replacing what’s missing: ceramides, cholesterol, and free fatty acids-in the right ratios.Research from the NIH and the Journal of Investigative Dermatology shows that formulations with a 1:1:1 ratio of ceramide:cholesterol:free fatty acids restore the skin’s natural lipid structure. These are called physiologic lipid replacements. In double-blind trials, they improved barrier function in 87% of users. Compare that to standard emollients-only 52% effectiveness.
Here’s what works:
- Ceramide-dominant creams: Look for products with 3-5% ceramides, 2-4% cholesterol, and 1-3% free fatty acids. Brands like CeraVe, EpiCeram, and TriCeram use this formula.
- pH 5.0-5.5: Your skin’s natural pH is slightly acidic. Products at this pH activate enzymes (β-glucocerebrosidase) that naturally build ceramides. At pH 7.0, those enzymes work at 40% efficiency. At pH 5.0? 90%.
- Applied right after bathing: The American Academy of Dermatology says applying moisturizer within 3 minutes of getting out of the shower traps 35% more moisture than waiting. Use 5 grams per arm (about two fingertip units).
What doesn’t work? Petroleum jelly alone. Fragranced lotions. Alcohol-based toners. And applying steroid creams on top of moisturizer without waiting 15 minutes. That’s a common mistake. Topical steroids can interfere with barrier repair if applied too soon. Wait. Then moisturize.
The Top Triggers You’re Probably Missing
You know sweat and stress trigger flares. But what about your laundry detergent? Your pillowcase? Your water hardness?Chronic eczema flares aren’t random. They’re triggered by things that damage the barrier or stir up inflammation. Here’s what actually matters:
- Hard water: Calcium and magnesium in tap water bind to soap, leaving residue that strips lipids. Install a shower filter if you live in Austin, Dallas, or any area with water over 120 ppm hardness.
- Detergents and fabric softeners: Even "hypoallergenic" ones can contain surfactants that irritate. Switch to fragrance-free, dye-free detergents like All Free & Clear or Tide Free. Wash clothes twice if you’re sensitive.
- Temperature swings: Cold air dries skin. Hot showers strip lipids. Keep showers under 10 minutes at 98-100°F. Use a humidifier in winter-aim for 40-50% humidity indoors.
- Staph aureus: This bacteria thrives on broken skin. Barrier repair reduces its presence by 65-75%. Bleach baths (½ cup in full tub, 10 minutes twice a week) help, but only if your barrier is already being repaired. Otherwise, it just burns.
- Overwashing: Washing your face or body more than once a day with soap? You’re removing natural oils. Use water only or a gentle cleanser like Cetaphil Gentle Skin Cleanser.
One Reddit user, u/EczemaWarrior, tracked their TEWL for 30 days after switching to a ceramide cream and avoiding fabric softener. Their TEWL dropped from 38 to 15 g/m²/h. Flares went from weekly to once a month. That’s not luck. That’s trigger control.

How to Stop the Itch-Without Steroids
The itch is the worst part. It’s not just annoying-it’s exhausting. You scratch because it feels good for a second. Then the skin breaks. Then it gets infected. Then it itches more. It’s a cycle.There are three ways to break it:
- Repair the barrier: When the skin is intact, nerve endings aren’t exposed. That alone cuts itch by 50-70% in most users.
- Cool it down: Cold compresses, chilled gel packs, or even a bag of frozen peas wrapped in a towel applied for 10 minutes can numb the itch. Avoid ice directly on skin.
- Use non-steroidal options: Pimecrolimus 1% cream (Elidel) doesn’t thin skin like steroids. It works by calming the immune response without damaging the barrier. Tacrolimus (Protopic) is another option. Both are prescription, but they’re safer for long-term use on the face and folds.
Some people swear by capsaicin cream (from chili peppers) to desensitize nerves, but it burns like hell at first. Not recommended unless you’re desperate. Antihistamines like Benadryl don’t work for eczema itch-they target allergic histamine, not neurogenic itch. Save them for allergies, not eczema flares.
Cost, Compliance, and Real-World Hurdles
Let’s be honest: barrier repair creams cost more. A 200g tube of CeraVe Healing Ointment runs $12. A prescription ceramide cream like EpiCeram? $85. Insurance covers prescription ones if you have a diagnosis, but over-the-counter? Not so much.That’s why 62% of users on MyEczemaTeam say they can’t afford it long-term. But here’s the math: if you’re using steroid creams every week, you’re paying for doctor visits, side effects, and lost productivity. One 2023 case study showed a 7-year-old reduced steroid use by 80% after 12 weeks of barrier repair. That’s savings.
And compliance? 85% of people learn the right technique within two weeks. But 40% quit because the cream feels greasy. That’s the texture hurdle. Solution? Try lighter formulations like CeraVe Moisturizing Cream (non-greasy) or Vanicream Moisturizing Skin Cream. Apply it while skin is still damp. Let it absorb for 10 minutes before dressing.
And if you have a severe filaggrin mutation? Barrier repair alone might not be enough. Studies show 30-40% of severe cases need help from JAK inhibitors like upadacitinib or abrocitinib. These are oral meds that calm the immune system. They’re not first-line, but they’re life-changing when barrier repair hits a wall.

What’s Next for Eczema Treatment
The future is personal. Companies like Dermavant are partnering with 23andMe to match barrier repair products to your filaggrin mutation type. If you have a null mutation, you’ll get a higher ceramide formula. If you have a partial one, you’ll get something with added moisturizing factors. Algorithms are already predicting product success with 85% accuracy.There’s also emerging research on platelet-rich plasma (PRP) injections-yes, from your own blood-to stimulate filaggrin production. Early studies show a 300% increase in filaggrin expression after one treatment. It’s experimental, but promising.
And sustainability? The EU is forcing manufacturers to use 30% biodegradable ingredients by 2027. Silicones and plastics in creams? Being phased out. You’ll see more plant-based ceramides, oat extracts, and algae-derived lipids.
By 2030, barrier repair will make up half of all eczema treatment. Right now, it’s 35%. The science is clear. The tools are here. The only thing missing is consistency.
Simple Daily Routine That Works
You don’t need 10 steps. You need three:- Morning: Wash face/body with water or gentle cleanser. Pat dry. Apply ceramide cream. Wait 10 minutes. Apply sunscreen (mineral-based, fragrance-free).
- Night: Lukewarm shower (no scrubbing). Pat dry. Apply ceramide cream immediately. Cover with cotton gloves or socks if hands/feet are cracked.
- Weekly: Bleach bath (twice a week) if you have frequent infections. Switch laundry detergent if you notice flares after washing.
That’s it. No magic. No expensive gadgets. Just repair, protect, repeat.
Can I use Vaseline for chronic eczema?
Vaseline (petrolatum) can help seal in moisture, but it doesn’t repair the skin barrier. It’s like putting tape over a leaky pipe-it stops water from escaping for now, but doesn’t fix the crack. For long-term healing, you need ceramides, cholesterol, and fatty acids. Use Vaseline only as a backup if your ceramide cream runs out.
Why does my eczema cream sting when I apply it?
Stinging usually means your skin barrier is severely damaged or you have open cracks. Barrier repair creams are often slightly acidic (pH 5.0-5.5) to activate repair enzymes, and that can burn on broken skin. Try applying a thin layer of petrolatum first, wait 10 minutes, then apply the ceramide cream. If it still stings after a week, switch to a neutral pH product like Vanicream.
How long until I see results from barrier repair?
You’ll feel less tightness and dryness in 7-10 days. But real barrier repair takes 28-42 days. That’s when the lipid layers rebuild and TEWL drops significantly. Don’t stop after two weeks. Stick with it. Studies show 92% compliance is needed for major improvement.
Are natural oils like coconut or olive oil good for eczema?
No. Coconut oil can worsen eczema in up to 30% of people because it contains lauric acid, which disrupts the skin’s natural lipid structure. Olive oil is too alkaline (pH 8) and damages the acid mantle. Stick to clinically tested ceramide formulas. Natural doesn’t mean better.
Can children use barrier repair creams?
Yes. In fact, early use in high-risk infants (those with a family history of eczema or asthma) can reduce flare risk by up to 50%. Use fragrance-free, pediatric-tested ceramide creams like CeraVe Baby Moisturizing Cream. Apply twice daily from birth if recommended by your pediatrician.
What to Do If It’s Not Working
If you’ve been doing barrier repair for 12 weeks with no improvement:- Get tested for filaggrin mutations (through 23andMe or a dermatologist).
- Check if you’re using too much product. Over-applying can clog pores and cause irritation.
- Rule out contact allergies with a patch test from a dermatologist.
- Consider a JAK inhibitor if flares are severe and frequent.
Chronic eczema isn’t cured overnight. But it’s controlled-with the right strategy. Fix the barrier. Avoid the triggers. Silence the itch. Do it every day. And for the first time in a long time, your skin might actually thank you.