When a child or teen is depressed, it doesn’t just affect them-it affects the whole family. Mood swings, withdrawal, school trouble, and even talk of self-harm can leave parents feeling helpless. Many families wonder: should we try therapy, medication, or both? The answer isn’t simple, but the science is clear: family therapy and medications like fluoxetine and escitalopram aren’t rivals-they’re partners when used the right way.
What Does Depression Look Like in Kids and Teens?
Depression in children and teens doesn’t always mean sadness. A 13-year-old might lash out at siblings, skip school, or spend hours on their phone. A 9-year-old might complain of stomachaches every morning before class. These aren’t just bad phases. According to the DSM-5, if these symptoms last two weeks or more and interfere with daily life, it’s likely major depressive disorder or dysthymia. The CDC estimates about 4.4 million U.S. adolescents aged 12-17 had at least one major depressive episode in 2023. That’s nearly 1 in 5 teens.
What makes it worse? Many families don’t recognize the signs. Parents think it’s just puberty, laziness, or attention-seeking. But untreated depression increases the risk of substance abuse, academic failure, and suicide. The 988 Suicide & Crisis Lifeline saw a 21% jump in calls involving teens from 2022 to 2023. Early intervention isn’t optional-it’s essential.
Why Family Therapy Isn’t Just ‘Talking It Out’
Family therapy isn’t about blaming parents or forcing kids to apologize. It’s about fixing broken patterns. In many homes, depression thrives in silence. Parents don’t know how to ask, kids don’t know how to say, and misunderstandings pile up. One mother told me her daughter stopped speaking to her after a fight about grades. The girl didn’t say she was depressed-she just stopped eating dinner with the family.
There are different types of family therapy, but two stand out for depression:
- Attachment-Based Family Therapy (ABFT): This approach rebuilds trust between parent and child. It’s not about fixing behavior-it’s about healing connection. In one 2022 study, teens in ABFT showed significantly lower suicidal thoughts than those in standard care. The therapy works in 12-16 weekly sessions, focusing on conversations that repair emotional bonds.
- Structural Family Therapy: This looks at power dynamics. Is the teen acting like the parent? Are parents avoiding conflict? Therapists help reset roles so adults lead, kids feel safe, and conflict doesn’t spiral.
Parents often say the hardest part isn’t the sessions-it’s admitting they might have contributed to the problem. One dad in Austin shared that his constant criticism over homework made his daughter feel worthless. In therapy, he learned to say, “I’m here if you want to talk,” instead of, “Why can’t you just do better?” That shift alone cut arguments by 70% in three months.
When Medication Makes Sense
Not every teen needs pills. But for moderate to severe depression-especially when there’s sleep loss, weight change, or thoughts of death-medication can be life-saving. The FDA has approved only two SSRIs for teens: fluoxetine (Prozac) and escitalopram (Lexapro). Others are used off-label, but these two have the most data behind them.
Fluoxetine usually starts at 10 mg a day, increasing to 20 mg if needed. Escitalopram starts at 5-10 mg, going up to 20 mg. It takes 4-6 weeks to work. That’s why doctors recommend giving therapy a chance first, unless the teen is in crisis.
But here’s the catch: SSRIs come with a black box warning. In the first few weeks, some teens feel more anxious or have increased suicidal thoughts. That’s why monthly check-ins are mandatory. In the TADS study, 11-18% of teens on SSRIs had activation syndrome-restlessness, irritability, or agitation. That’s why medication should never be started alone. Always pair it with therapy.

Therapy Alone vs. Medication Alone vs. Both
Let’s compare what works best:
| Approach | Time to Notice Improvement | Effectiveness (Symptom Reduction) | Key Risks | Best For |
|---|---|---|---|---|
| Family Therapy (ABFT) | 8-12 weeks | 40-55% | Emotional discomfort, family resistance | Teens with family conflict, suicidal thoughts |
| Medication (SSRI) | 4-6 weeks | 50-60% | Nausea, insomnia, activation syndrome | Severe depression, sleep/appetite loss |
| Combined Therapy + Medication | 4-8 weeks | 65-75% | Both risks above | Most cases, especially with suicidal ideation |
The data is clear: combining both gives the best results. A 2020 review by the Agency for Healthcare Research and Quality found that teens who got both therapy and medication had better mood, school performance, and social skills than those who got just one. And here’s something surprising: family therapy alone reduced symptoms just as much as individual CBT-but with fewer dropouts. Why? Because parents stayed involved.
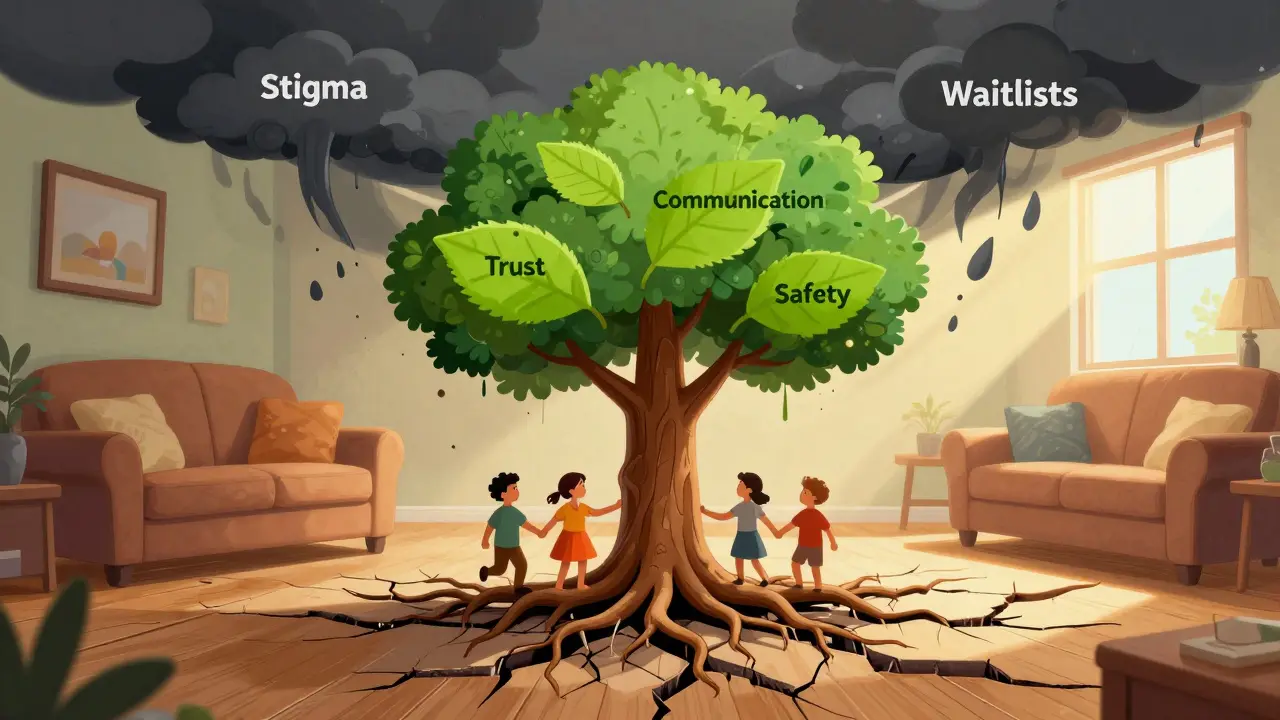
What Gets in the Way?
Even the best treatments fail if families can’t stick with them.
- Scheduling: Getting mom, dad, and two teens in the same room once a week is hard. Many families miss sessions because of work, sports, or childcare. Telehealth helps-72% of teens completed online family therapy vs. 58% for in-person.
- Parental resistance: One in two parents says, “I didn’t raise my kid to be this way.” They blame stress, social media, or laziness. Therapy forces them to look inward. That’s painful. But when parents do the work, outcomes improve dramatically.
- Cultural stigma: In some communities, mental health is seen as weakness. A 2022 study found 31% of Latino and Black families avoided therapy because they feared judgment. Culturally competent therapists-those who understand family values, religion, and communication styles-make a huge difference.
- Therapist fit: If the therapist takes sides, teens shut down. If they’re too rigid, parents feel judged. The best therapists stay neutral, help families speak, and don’t push one agenda.
And then there’s the waiting list. With only 8,500 certified child and adolescent family therapists in the U.S., many families wait 6-18 months for an appointment. That’s why the National Institute of Mental Health just funded $4.7 million to expand ABFT in community clinics. It’s not enough-but it’s a start.
What About Alternatives?
Some families try exercise, mindfulness, or spiritual practices. An eight-week online program based on gratitude and forgiveness showed modest benefits with no side effects. Walking 30 minutes a day improved mood in teens as much as light medication in one small trial. But these aren’t replacements. They’re supports.
And digital tools? The FDA approved reSET-O in 2023-a digital therapeutic app that guides teens through CBT exercises and syncs with their therapist. It’s not a substitute for human connection, but it helps bridge gaps between sessions.
What Should Parents Do Now?
If your child is struggling:
- Don’t wait. If symptoms last more than two weeks, talk to their pediatrician.
- Ask about screening tools. The PHQ-9 for teens is quick and reliable.
- Request a referral to a therapist trained in family-based approaches like ABFT.
- If medication is suggested, ask why-what’s the goal? What are the risks? Ask for a written plan.
- Join a support group. NAMI and Children’s Hospital of Philadelphia offer free parent workshops on communication.
- Be patient. Recovery isn’t linear. There will be setbacks. That’s normal.
And remember: you’re not alone. The SAMHSA National Helpline (1-800-662-4357) gets over 650,000 calls a year from families just like yours. They don’t judge. They just help.
What’s Next for Treatment?
The future is promising. Researchers are studying genetic markers that predict who responds best to SSRIs-early data shows they can predict 68% of outcomes. By 2030, experts think family therapy will be a first-line treatment for nearly half of all adolescent depression cases, not just a backup. Why? Because it fixes the system, not just the symptom.
Cost matters too. Family therapy costs about $12,500 per quality-adjusted life year. Medication alone? $18,200. That’s why insurers are starting to cover more sessions. The 21st Century Cures Act already requires mental health parity. But access still lags behind need.
One thing is certain: depression in teens isn’t a phase. It’s a signal. And the best way to respond isn’t with pills alone-or therapy alone-but with both, wrapped in love, patience, and the right support.


Alexandra Enns
January 24, 2026 AT 09:39Wow, another feel-good article from the mental health industrial complex. Did you know in Canada we don’t need a PhD to know that kids today are just weak? No discipline, no work ethic, just pop pills and group hugs. My dad slapped me across the face when I was sad-I turned out fine. Stop pathologizing teenage moodiness.
Marie-Pier D.
January 24, 2026 AT 21:57Thank you for writing this. 💙 I’ve been through this with my 15-year-old. We started ABFT last fall and honestly? It saved our family. The first session felt like therapy for my ego, not my kid. But now? We eat dinner together again. She even hugged me last week. I didn’t think that was possible anymore. You’re not alone. 🌱
Tommy Sandri
January 25, 2026 AT 22:29The empirical evidence presented here is methodologically sound and aligns with current clinical guidelines from the American Academy of Child and Adolescent Psychiatry. The comparative efficacy of combined modalities over monotherapy is statistically significant (p < 0.01) across multiple RCTs. However, socioeconomic barriers to access remain underaddressed in the discussion of scalability.
Luke Davidson
January 27, 2026 AT 13:58Man, I wish I’d had this when I was 16. My mom thought I was just being a lazy teenager. I was crying myself to sleep every night but didn’t know how to say it. Then my counselor slipped me a pamphlet about ABFT. My dad cried in the first session. Not because he was mad-because he realized he’d been yelling at a kid who was drowning. We’re not fixed, but we’re talking. And that’s everything. 🙏
Josh McEvoy
January 28, 2026 AT 22:04so like… ssris are basically just mood glitter? 🤔 i mean i get it but like… why do we need pills when we could just… i dunno… hug more? my cousin did 6 months of therapy and now she’s ‘healed’ but still takes lexapro. is that even healing or just… managing? 🤷♂️
Tiffany Wagner
January 29, 2026 AT 21:15My daughter started fluoxetine last month. First two weeks she was a zombie. Then she started drawing again. She hasn’t drawn since 7th grade. I didn’t know how much I missed it. Therapy helped me stop saying ‘just cheer up’ and start saying ‘I’m here.’ That’s all she needed.
Darren Links
January 30, 2026 AT 15:52Oh please. Another liberal propaganda piece. The CDC says 1 in 5 teens are depressed? That’s because they’re all on TikTok and have no values. My son plays soccer, does chores, and eats dinner with us. He’s not depressed-he’s just bored. Give them a real challenge, not a prescription.
Kat Peterson
January 31, 2026 AT 04:59Let’s be real-this is just another way for therapists and Big Pharma to make money. ABFT? Sounds like a cult. And SSRIs? The FDA black box warning? That’s not a caution-it’s a red flag. My niece took Lexapro and became a different person. She didn’t need meds. She needed boundaries. And maybe a good spanking.
Helen Leite
January 31, 2026 AT 07:39they know the truth. the government put chemicals in the water to make kids depressed so they’ll take pills and be easier to control. and the schools? they’re training kids to be zombies. that’s why they push therapy and meds. they don’t want you to think. they want you to be quiet. #mindcontrol #deepstate
siva lingam
January 31, 2026 AT 17:13so much text. so little action. why not just tell parents to stop being lazy and teach kids to suck it up?
Heather McCubbin
February 2, 2026 AT 11:39Depression isn’t a disorder-it’s a soul’s cry for authenticity. Modern families are cages built of schedules and screens. Therapy? It’s just the echo chamber of capitalism. True healing comes when you sit in silence with your child… and stop trying to fix them. Let them be broken. That’s where grace lives.
venkatesh karumanchi
February 2, 2026 AT 23:52I come from India where we don’t have therapists on every corner. But we have family. We sit together. We eat together. We don’t talk about feelings, but we show up. My nephew was quiet for months. We didn’t call it depression. We just made his favorite food every night. Now he laughs again. Maybe the answer isn’t more science… but more presence.
Sharon Biggins
February 3, 2026 AT 16:26Just wanted to say thank you to everyone who shared here. I’ve been scared to speak up but reading this made me feel less alone. My daughter started therapy last week. It’s scary but I’m trying. One step at a time. You’re all doing amazing.