Antihistamine Reaction Risk Assessment Tool
Antihistamine Reaction Assessment
This tool helps you determine if your symptoms might be due to a paradoxical antihistamine reaction, where the medication makes your allergic symptoms worse instead of better.
Important: This assessment tool is for informational purposes only. If you're experiencing severe allergic reactions to antihistamines, please seek immediate medical attention. Consult with an allergist for proper diagnosis and treatment.
It’s ironic, isn’t it? You take an antihistamine because you’re itching, sneezing, or breaking out in hives - and instead of feeling better, your skin gets worse. You’re not imagining it. Some people have antihistamine allergies - a rare but real condition where the very drugs meant to stop allergic reactions end up causing them.
How Can a Medication Cause the Problem It’s Supposed to Fix?
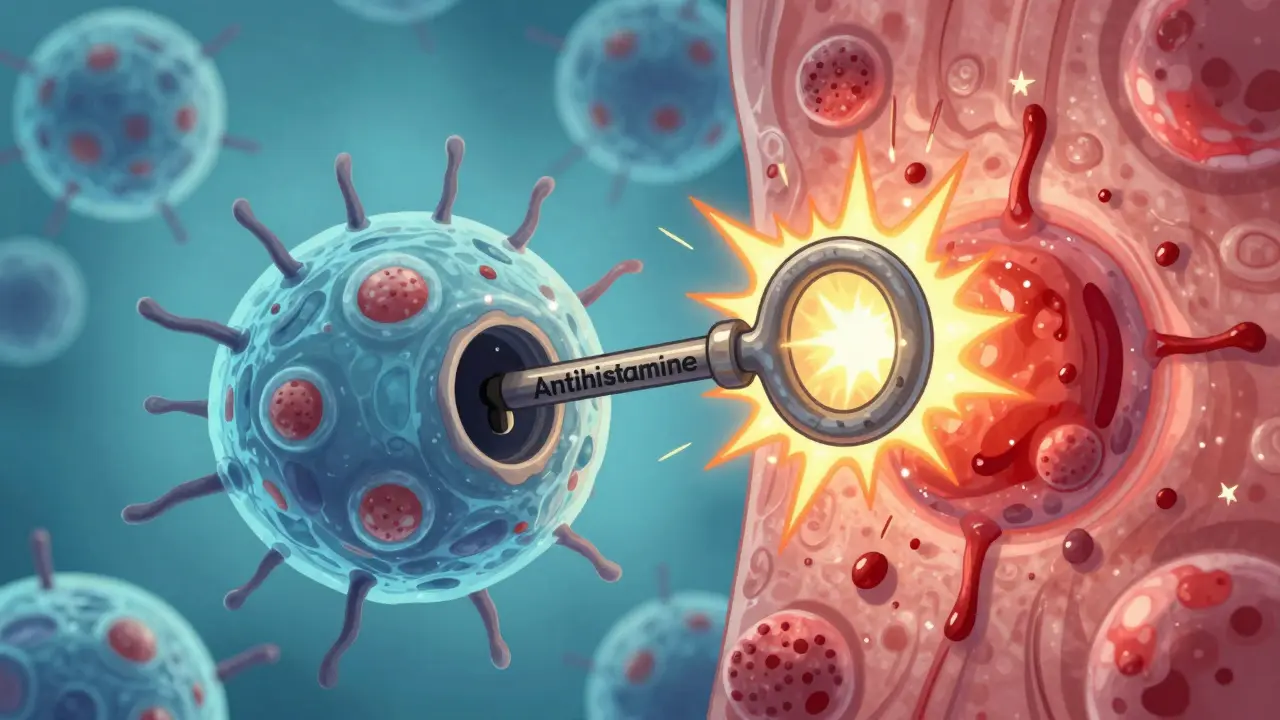
Most antihistamines work by blocking histamine from binding to H1 receptors on your cells. Histamine is the chemical your body releases during an allergic reaction. It’s what makes your nose run, your eyes water, and your skin swell. Antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and diphenhydramine (Benadryl) were designed to sit in those receptor spots and prevent histamine from triggering symptoms. But in a small number of people, something strange happens. Instead of blocking the receptor, the antihistamine actually turns it on. Think of it like a key that fits the lock but accidentally turns it the wrong way. Researchers call this paradoxical activation. A 2017 case study published in Allergol Select followed a woman who developed worsening hives every time she took any common antihistamine - even ones she’d used safely before. Her symptoms only went away after she stopped all antihistamines and treated an underlying chronic infection. That’s when doctors realized: her body wasn’t reacting to the drug as an allergen - it was reacting to how the drug changed the shape of the receptor. Cryo-EM imaging from a 2024 study in Nature Communications showed that antihistamines normally bind deep inside the H1 receptor, locking it in an inactive state. But in hypersensitive individuals, the drug’s structure might stabilize the receptor in its active form - the exact opposite of what it’s supposed to do. The same drug that calms your allergies in most people can set off a flare-up in others.Which Antihistamines Are Most Likely to Cause Problems?
You might assume that if one antihistamine causes a reaction, others in the same class will too. But it’s not that simple. There are two main types: first-generation and second-generation. First-generation antihistamines - like diphenhydramine, chlorpheniramine, and pheniramine - cross the blood-brain barrier. That’s why they make you sleepy. They also block other receptors, like muscarinic ones, which can cause dry mouth, blurred vision, and urinary retention. In rare cases, they’ve triggered immediate allergic reactions, including anaphylaxis. One documented case involved pheniramine causing a severe reaction in someone with multiple drug hypersensitivity syndrome. Second-generation antihistamines - like fexofenadine, loratadine, cetirizine, and desloratadine - were developed to be less sedating. They stay mostly outside the brain and last longer (12-24 hours). But here’s the twist: they’re just as likely to cause paradoxical reactions. The same 2017 study found that patients reacted to both piperidine-based drugs (fexofenadine, loratadine) and piperazine-based ones (cetirizine, hydroxyzine). That means even if you’ve tried one type and it didn’t cause a problem, another - even from a different chemical group - might. A 2018 case in the Korean Journal of Pediatrics showed a child who had negative skin tests for ketotifen (a less common antihistamine) but broke out in hives after taking it orally. The reaction didn’t happen right away - it took 120 minutes. That’s why skin tests alone aren’t enough.Why Skin Tests Often Miss the Problem
Doctors often rely on skin prick tests to check for allergies. You get a tiny drop of the drug on your skin, a little poke, and wait for a welt. If there’s no reaction, the drug is considered safe. But with antihistamine hypersensitivity, that’s not reliable. Skin tests look for IgE-mediated reactions - the classic allergic response. But paradoxical activation isn’t IgE-driven. It’s a receptor-level glitch. So you can have a perfectly normal skin test and still get hives after swallowing the pill. The only way to be sure? An oral challenge - taking the drug under medical supervision and watching closely for symptoms. This is risky, which is why it’s only done in controlled settings. But if you’ve had repeated unexplained hives that don’t respond to antihistamines, this might be your only path to answers.
What to Do If You Think You’re Reacting to Antihistamines
If you’ve taken an antihistamine and your symptoms got worse - more itching, new hives, swelling, or even trouble breathing - stop taking it immediately. Don’t assume it’s just your allergy flaring up. That’s what happened to the patient in the 2018 case. Her doctors thought she had chronic urticaria. It took months to realize the antihistamine was the trigger. Here’s what to do next:- Keep a symptom diary. Note every medication you take and when your skin reacts. Include timing - did the reaction happen 30 minutes after taking it? Or 2 hours?
- Stop all antihistamines. This includes OTC ones like Benadryl, Zyrtec, and even allergy eye drops or topical creams.
- See an allergist who’s familiar with drug hypersensitivity. Not all allergists know about paradoxical reactions. Ask if they’ve seen cases like this before.
- Ask about underlying triggers. In the 2017 case, treating a chronic infection cleared the hives. Other triggers can include viruses, stress, or autoimmune conditions.
What Are Your Alternatives If You Can’t Take Antihistamines?
If antihistamines are off the table, you still have options - but they’re not as simple as popping a pill.- Leukotriene inhibitors like montelukast (Singulair) can help with allergy symptoms without touching H1 receptors. They’re often used for asthma but also reduce nasal congestion and hives in some patients.
- Omalizumab (Xolair) is an injectable biologic approved for chronic spontaneous urticaria. It targets IgE directly and works even when antihistamines fail. It’s not cheap, but for people who’ve tried everything else, it can be life-changing.
- Immunosuppressants like cyclosporine may be used short-term in severe cases, though they come with side effects and need monitoring.
- Non-drug approaches like cold compresses, loose clothing, avoiding heat and sweating, and stress reduction can help manage symptoms while you figure out the root cause.
And remember - H2 antihistamines like famotidine (Pepcid) work on a different receptor (H2), mostly in the stomach. They don’t help with hives or runny nose, but they’re not cross-reactive with H1 blockers. So if you’re reacting to Zyrtec or Claritin, Pepcid won’t make it worse.

The Bigger Picture: Why This Matters
Antihistamines are among the most common medications in the world. Millions take them every day. But when they backfire, the consequences can be serious - especially if you keep taking them, thinking it’s just your allergy getting worse. The fact that this reaction can happen across different chemical classes means you can’t assume safety just because you’ve tolerated one type. It also means that future drug development needs to account for receptor polymorphisms - genetic differences that make some people respond differently to the same molecule. Researchers are already using those cryo-EM structures to design new antihistamines that avoid the paradoxical activation trap. One study even identified a secondary binding site on the H1 receptor that could be targeted to create safer drugs. That’s promising. But for now, if you’re one of the rare people affected, the best advice is simple: listen to your body. If an antihistamine makes you worse, it’s not in your head. It’s in your receptors.When to Call Your Doctor
You don’t need to panic if you’ve had a mild reaction. But call your doctor if:- Your hives or swelling get worse after taking an antihistamine
- You’ve tried multiple antihistamines and none help - or they all make things worse
- You develop swelling in your lips, tongue, or throat
- You feel dizzy, short of breath, or your heart races after taking the medication
These could be signs of a more serious reaction - and you need help fast.
Can you be allergic to antihistamines even if you’ve taken them before without problems?
Yes. Allergic reactions to antihistamines aren’t always immediate or predictable. Some people develop paradoxical hypersensitivity over time, especially if they have an underlying condition like chronic infection or autoimmune disease. Even if you’ve used cetirizine or loratadine safely for years, your body’s receptors can change how they respond - leading to new reactions.
Do all antihistamines cross-react with each other?
Not always, but they can. While antihistamines come in different chemical classes - piperidines like fexofenadine and piperazines like cetirizine - patients with hypersensitivity often react to multiple types. One study showed a person reacting to both first- and second-generation drugs, even when they had different structures. That’s why avoiding all antihistamines is often necessary until you get tested properly.
Why do skin tests sometimes give false negatives for antihistamine allergies?
Skin tests detect IgE-mediated allergies - the kind that cause immediate hives or anaphylaxis. But antihistamine hypersensitivity is usually a receptor-level issue, not an IgE response. That means your skin might show no reaction, yet you still get hives after swallowing the pill. Oral challenges are the only reliable way to confirm this type of reaction.
Are there any antihistamines that are safer for people with this issue?
No. Because the reaction isn’t about the drug’s chemical structure alone - it’s about how your H1 receptors respond - there’s no guaranteed safe option among H1 blockers. Even newer drugs like bilastine or rupatadine carry the same risk. The safest approach is complete avoidance until you’ve been evaluated by a specialist.
Can treating an infection help with antihistamine-induced hives?
Yes. In at least one documented case, a patient’s chronic hives disappeared only after treating a hidden bacterial infection. Researchers believe chronic inflammation can make H1 receptors more sensitive to paradoxical activation. If you’ve been struggling with unexplained hives and antihistamines aren’t helping, ask your doctor about testing for infections like H. pylori, hepatitis, or even Lyme disease.

Vu L
December 28, 2025 AT 09:14So let me get this straight - the drug that’s supposed to stop your allergies turns your body into a walking allergy factory? That’s like buying a fire extinguisher and it sets your house on fire. I’ve been on Zyrtec for years, and now you’re telling me it’s secretly sabotaging me? Cool. Cool cool cool. I’m switching to just breathing through a paper bag from now on.
James Hilton
December 29, 2025 AT 15:17Bro, if your body hates antihistamines, maybe your body’s just mad you’re treating allergies like a vending machine snack. Like, chill. Let your immune system have a damn nap. Also, have you tried not being allergic to everything? Just a thought.
Mimi Bos
December 31, 2025 AT 05:45i had this happen once with benadryl and thought i was going crazy lol. my face got all red and itchy and i was like ‘but this is supposed to help??’ then i stopped it and it went away. weird right? also i keep typing ‘antihistamine’ as ‘antihistimine’ 😅
Payton Daily
January 1, 2026 AT 06:09Think about it. The human body isn’t a machine. It’s a cosmic glitch in a universe that doesn’t care if you sneeze or not. Antihistamines? They’re just little chemical ghosts trying to boss around your receptors like they own the place. But your cells? They remember. They rebel. And when they do - ohhh, the gods of immunology laugh. This isn’t medicine. This is a war between your molecules and your soul. You think you’re treating an allergy? No. You’re negotiating with your own biology - and sometimes, your biology says ‘nope.’
Kelsey Youmans
January 1, 2026 AT 22:30Thank you for this comprehensive and clinically nuanced exploration. It is both enlightening and deeply reassuring to encounter such rigorous attention to the biological mechanisms underlying paradoxical drug responses. The distinction between IgE-mediated hypersensitivity and receptor-level dysregulation is critical, and I appreciate the emphasis on the necessity of supervised oral challenges in diagnostic confirmation. This represents a vital contribution to patient safety and pharmacological literacy.
Sydney Lee
January 2, 2026 AT 06:49Let me be clear: if you’re reacting to antihistamines, you’re either genetically inferior or you’ve been poisoning your body with processed sugar and social media for too long. Real people don’t have ‘paradoxical activation’ - they have weak immune systems and poor lifestyle choices. Also, why are you taking antihistamines in the first place? Go outside. Touch grass. Stop being a lab rat for Big Pharma.
oluwarotimi w alaka
January 3, 2026 AT 15:54usa medicales be trippin. in nigeria we just use neem leaves and pray. why you people always need pills for everything? this antihistamine thing? its a western scam to sell more drugs. even your doctors dont know what they doing. i heard they put microchips in the pills now to track you. why you think they want you to take it all the time? its not allergy… its control.
Debra Cagwin
January 4, 2026 AT 06:31If you’ve experienced this, please know you’re not alone - and you’re not broken. Your body is communicating with you, even if the message is confusing. It’s okay to stop what’s making you worse. It’s okay to ask for help. There are alternatives, and there are doctors who will listen. You’re doing the right thing by paying attention to your body. Keep going. You’ve got this 💪❤️
Hakim Bachiri
January 6, 2026 AT 04:42Okay so let me get this straight - the drugs are so advanced they can flip your receptors like a switch? That’s wild. But also… who approved this? I mean, if a drug can literally reverse its own function based on your DNA, then we’re not treating allergies - we’re playing god with a blindfold on. And don’t even get me started on the fact that the FDA lets this stuff out into the wild like it’s a free sample at Costco. Someone’s getting rich off this. Not you. Not me. Someone in a suit with a yacht.
Celia McTighe
January 8, 2026 AT 02:06OMG this is SO relatable 😭 I had this happen with Claritin and I thought I was losing my mind! I cried in the pharmacy aisle because I just wanted to stop sneezing and instead I looked like I’d been stung by 100 bees. Thank you for writing this - I feel less alone now. 🫂 Also, cold compresses are LIFE. I keep ice packs in my freezer just for this 😅
Ryan Touhill
January 8, 2026 AT 13:06It’s fascinating how modern pharmacology has become a paradoxical art form - where the cure becomes the disease, and the diagnostic tools are blind to the very mechanism they’re meant to detect. The H1 receptor isn’t just a protein; it’s a mirror of our genetic fragility. And yet, we continue to treat it like a broken faucet, turning the knob harder until it bursts. We need not just better drugs - we need humility. The body doesn’t obey formulas. It remembers. It adapts. It resists. And in that resistance, perhaps, lies a deeper truth about medicine itself: we don’t control it. We merely observe it. And sometimes… we’re the ones who need healing more than the patient.