Swelling in your lips, tongue, or throat after starting a blood pressure pill? It might not be an allergy. It could be something far more dangerous - and far more common - than most doctors realize. ACE inhibitor-induced angioedema is a silent, life-threatening reaction that can strike even after years of safe use. And the worst part? Most emergency rooms still treat it like a regular allergic reaction - with antihistamines and epinephrine - which do absolutely nothing.
What Exactly Is ACE Inhibitor Angioedema?
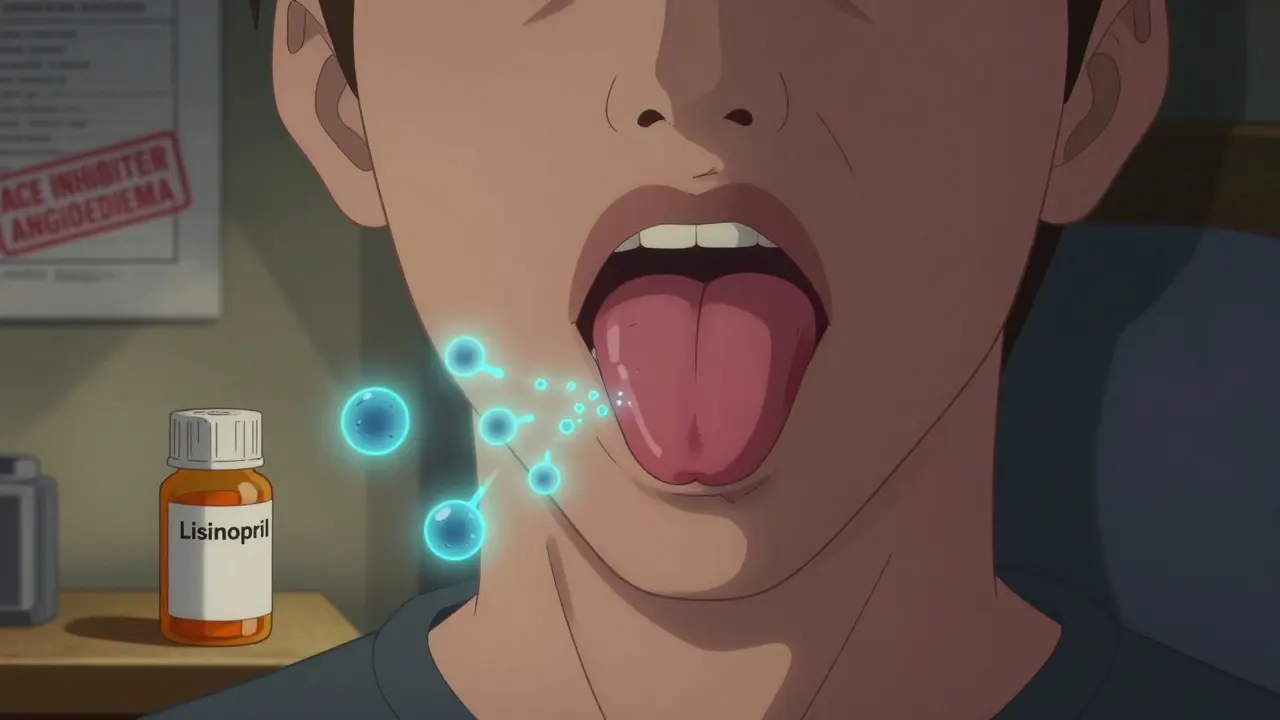
ACE inhibitors are among the most prescribed drugs in the U.S., used to treat high blood pressure, heart failure, and kidney disease in millions of people. Common ones include lisinopril, enalapril, and ramipril. But for about 1 in 200 people taking them, these drugs trigger a sudden, painless swelling - usually in the face, lips, tongue, or throat. This isn’t hives. It’s not itchy. It doesn’t come with a rash. That’s why it’s so often missed.
The real culprit? Bradykinin. ACE inhibitors block the enzyme that breaks down this peptide. When bradykinin builds up, it leaks fluid into tissues, causing swelling. Unlike allergic reactions, which involve histamine, this is a completely different biological pathway. That’s why Benadryl, steroids, and epinephrine don’t work. Giving them is like trying to put out a gasoline fire with water.
Who’s at Risk?
This isn’t random. Certain groups are far more likely to develop it. African Americans face a 2 to 4 times higher risk than other ethnic groups. Women are affected twice as often as men. And while it can happen anytime, half of all cases show up within the first week of starting the drug. But here’s the twist: 20% of cases happen after 10 or more years of safe use. One patient in a medical journal developed swelling after 15 years on lisinopril - no prior issues, no warning.
There’s also a dangerous combo: taking an ACE inhibitor with a DPP-4 inhibitor for diabetes (like sitagliptin or saxagliptin). That combination increases your risk by 4 to 5 times. If you’re on both, you need to be extra vigilant.
Why Emergency Rooms Get It Wrong
Most ER doctors are trained to think of swelling as an allergic reaction. They reach for epinephrine, diphenhydramine, and steroids. But multiple studies - including those from the EMCrit podcast, DermNet, and the MSD Manual - confirm these treatments have zero effect on ACE inhibitor angioedema. In fact, they delay the right care.
One patient on Reddit shared how he went to the ER three times over two weeks. Each time, he got epinephrine and Benadryl. Each time, the swelling came back. Only after insisting on a specialist consult did someone finally say: “Stop the lisinopril.” Within 48 hours, it started to fade.
That’s not rare. A 2022 study in the Journal of Emergency Medicine found that 55% of ER doctors misdiagnose this condition on the first visit. Patients average 2.3 emergency visits before getting the correct diagnosis. And each visit costs $1,850 on average. Hospitalization for airway complications? That jumps to $7,200.
What Actually Works
The only guaranteed fix? Stop the ACE inhibitor - immediately and permanently. No exceptions. If you keep taking it, episodes will come back - and they’ll get worse. The American College of Emergency Physicians says every patient who survives one episode should get a medical alert bracelet. Your chart must clearly say “ACE inhibitor-induced angioedema - permanent contraindication.” Not “allergy.” Not “sensitivity.” That wording matters. Future doctors might otherwise prescribe another ACE inhibitor.
For severe cases where breathing is at risk, airway protection comes first. Intubation or a tracheostomy might be needed. But if the swelling isn’t blocking your airway yet, there are targeted treatments:
- Icatibant (Firazyr): A bradykinin blocker. Works in 2-4 hours. Costs about $9,000 per dose in the U.S.
- Ecallantide: Blocks kallikrein, the enzyme that makes bradykinin.
- C1-inhibitor concentrate: Used for hereditary angioedema, sometimes works here too.
- Fresh frozen plasma (FFP): Contains ACE enzyme. Used off-label in emergencies when other options aren’t available. Limited evidence, but some success in case reports.
None of these are first-line in most hospitals. But if you’ve had this reaction before, ask your doctor about keeping icatibant on hand. It’s expensive, but it saves lives.
What Comes Next?
Once you stop the ACE inhibitor, swelling usually fades within 24-48 hours. But for some, mild swelling lingers for months. One patient reported lip swelling for four months after stopping lisinopril. That’s normal. It doesn’t mean the drug is still active - it just means your body takes time to clear the excess bradykinin.
Switching to an ARB (angiotensin receptor blocker) like losartan or valsartan is the standard next step. ARBs don’t affect bradykinin the same way. Their angioedema risk is about 10 times lower. But here’s the catch: 10-15% of people who had ACE inhibitor angioedema will get it again on an ARB. So monitor closely. If swelling returns, stop it immediately.

Why This Isn’t Getting Better
Despite being one of the most common causes of drug-induced angioedema - making up about 30% of all ER cases - this condition is still underdiagnosed. The FDA added black box warnings to ACE inhibitors in 2010. But warnings don’t change practice. A 2022 study found only 42% of patients who had an episode were properly counseled about avoiding ACE inhibitors forever. That’s a failure in patient safety.
Meanwhile, research is moving forward. A 2023 study in the Pharmacogenomics Journal found that a specific gene variant (XPNPEP2) increases risk by 3.7 times. That gene controls an enzyme that helps break down bradykinin. People with this variant are essentially born with a weaker backup system. In the next five years, experts predict genetic screening will become routine for high-risk groups - especially African Americans.
For now, the message is simple: If you’re on an ACE inhibitor and notice sudden swelling - especially in your face or throat - stop the drug and get help. Don’t wait. Don’t assume it’s just allergies. Don’t let them give you Benadryl and send you home. Ask: “Could this be ACE inhibitor angioedema?”
What You Need to Remember
- Swelling from ACE inhibitors is not an allergy. It doesn’t respond to epinephrine or antihistamines.
- It can happen anytime - even after 10+ years of use.
- African Americans and women are at higher risk.
- Combining ACE inhibitors with DPP-4 inhibitors increases risk 4-5 times.
- Stop the ACE inhibitor immediately. Never restart it.
- Switch to an ARB - but watch for recurrence.
- Get a medical alert bracelet if you’ve had a severe episode.
- Document it clearly in your medical records: “ACE inhibitor-induced angioedema - permanent contraindication.”
Every year, tens of thousands of people get this reaction. Many survive. Some don’t. The difference? Recognition. Speed. Knowing what to do - and what not to do.

Vince Nairn
January 7, 2026 AT 23:25So let me get this straight - we’re giving millions of people a drug that can silently choke them out years later, and the ER’s still treating it like a bee sting? 😅
My aunt took lisinopril for 12 years. One morning her lips looked like she’d been kissed by a balloon animal. They gave her Benadryl. She went home. Swelling came back. Twice. By the third time, she screamed until someone listened. Turns out - no allergy. Just bradykinin being a drama queen.
Why does this still happen? Because doctors are trained to see allergies, not biochemistry. It’s like teaching plumbers to fix computers because both have wires.
And yeah, that 55% misdiagnosis stat? I believe it. I’ve seen it. My cousin’s dad almost died because they kept giving him steroids. He was fine after they stopped the pill. No magic. Just stopping the poison.
Why isn’t this on every med sheet? Why isn’t every patient with ACE inhibitors handed a card that says ‘IF SWELLING - STOP THIS DRUG’? We’re not talking rare. We’re talking ‘your neighbor’s mom’ common.
And the cost? $1,850 per ER trip? That’s a luxury car. Imagine how many people could’ve been saved if we spent that money on education instead of triage chaos.
Also - icatibant costs $9,000? That’s insane. Why isn’t this a generic? Why isn’t it in every ambulance? We have epinephrine for peanut allergies. We need bradykinin blockers for this. It’s not optional. It’s basic.
And ARBs? 10-15% risk? That’s still too high. We need better alternatives. Not just ‘try this other pill and hope’. We need real science. Not luck.
Someone needs to make a viral video about this. Like, ‘What if your blood pressure pill could kill you silently?’
And yes - I’m now checking my own meds. Thanks for the wake-up call.
Aparna karwande
January 9, 2026 AT 10:26OMG this is exactly what happened to my uncle in Mumbai! He was on ramipril for 8 years - no issues. Then one day his tongue swelled like a balloon. Took him 4 hours to get to the hospital because traffic. They gave him antihistamines. He almost suffocated. Finally, a young resident - fresh from the U.S. - asked: ‘Did you take any blood pressure pills?’ He said yes. The doctor said: ‘STOP IT NOW.’ Swelling went down in 12 hours.
But here’s the kicker - the doctor who prescribed it? Never called him back. Never warned him. Just moved on to the next patient.
And now? They’re putting him on losartan. He’s scared. He says his heart feels like it’s holding its breath.
India needs a national campaign. Not just ‘take your pills’ - but ‘know what your pills can do’. This isn’t just medical. It’s cultural. We trust doctors too much. We don’t question. We swallow. Literally.
And why is this not in medical school curricula here? Why are we still teaching this like it’s 1995?
Someone needs to start a petition. #StopTheSilentKiller
Kamlesh Chauhan
January 10, 2026 AT 23:36Bro this is wild
i took lisinopril for 3 years and never had a problem but now i see people freaking out like its the end of the world
maybe its just me but i think most of this is just fearmongering
like yeah sure its rare but why are we acting like everyone on ACE inhibitors is gonna wake up with a face like a pufferfish
my grandpa took this for 20 years and died of a heart attack not a swollen tongue
maybe stop being so dramatic
also who even has 9000 dollars to spend on some fancy shot
we need cheaper solutions not more panic
Adam Gainski
January 12, 2026 AT 03:17Thank you for writing this with such clarity. I work in a rural ER and we get 2-3 suspected cases a month. Most of the time, we default to the allergy protocol because it’s what we’re taught, what’s in the protocol book, and what’s fast.
But after reading this - and a few patient stories - I started asking the simple question: ‘Are you on an ACE inhibitor?’
One patient, a 68-year-old woman, had swelling for three days. We gave her Benadryl twice. She came back. I asked again. She said yes, lisinopril. I stopped it. She left with a referral to cardiology. Two days later, she texted me: ‘My lip is back to normal.’
It’s not about being a hero. It’s about being curious. And sometimes, the most powerful thing you can do is stop doing what you’ve always done.
I’ve printed out a one-pager on ACE angioedema and taped it to the med cart. If you’re reading this - do the same. It takes 30 seconds. It might save a life.
Also - yes, the cost of icatibant is insane. But if we invested even 10% of what we spend on misdiagnoses into stocking it in regional ERs, we’d save money and lives. It’s not a luxury. It’s a public health gap.
Paul Mason
January 12, 2026 AT 20:52Look I’ve been a nurse for 20 years and I’ve seen this a dozen times. You think it’s complicated? It’s not.
Swelling? No rash? No itching? On a blood pressure pill? STOP THE PILLS. DONE.
Why do we make everything so hard? We have a checklist: 1. Drug? 2. Swelling? 3. No hives? 4. Then it’s ACE. Not allergy. Not asthma. Not stress. ACE.
And yeah, Icatibant? Expensive. But if you’re in the ER and your airway is closing - you don’t care about cost. You care about breathing.
My advice? If you’re on one of these drugs and you feel funny - stop it. Call your doctor. Don’t wait. Don’t Google. Don’t hope it goes away.
And if you’re a doctor - stop treating it like a rash. It’s not. It’s a silent bomb.
Simple. Done.
Katrina Morris
January 14, 2026 AT 19:01i just found out my mom is on lisinopril and she had a little swelling last month but thought it was from eating too much salt 😅
now im kinda freaking out
she’s 72 and her doctor just says ‘keep taking it’
should i bring this article to her next appt?
also what’s an arb? is it like a different kind of pill?
thank you for writing this i feel like i learned something today
steve rumsford
January 15, 2026 AT 19:58So I’ve been on enalapril for 7 years. No issues. But now I’m paranoid.
Yesterday I ate a mango and my lip tingled. I froze. Sat there for 20 minutes thinking I was about to die.
Turned out it was just the mango. But now I’m scared to eat fruit.
Also I just Googled ‘bradykinin’ and now I have nightmares.
Why does medicine feel like a horror movie sometimes?
Andrew N
January 17, 2026 AT 15:08Let’s be real. This is just another example of pharmaceutical oversight failing patients.
ACE inhibitors were approved in the 80s. The bradykinin link was known by the 90s. But no one changed the labeling. No one mandated patient education. No one funded research for alternatives.
Because profit > safety.
Big Pharma makes billions off these drugs. A single dose of lisinopril costs 12 cents. The patent expired. Generic prices are dirt cheap. So why bother fixing a problem that doesn’t affect profits?
Meanwhile, patients die quietly. ERs bill for useless treatments. Insurance pays. Everyone wins except the person with the swollen tongue.
It’s not negligence. It’s economics.
LALITA KUDIYA
January 17, 2026 AT 22:53i’m from india and my mom is on ramipril too
she never told me she had swelling once last year
she thought it was just allergies
now i’m going to talk to her
thank you for sharing this
we need more awareness here
❤️
Poppy Newman
January 18, 2026 AT 04:15OMG I didn’t know this was a thing 😱
I’ve been on lisinopril for 5 years and I’ve had ‘weird lip swelling’ twice - thought it was stress or food
I’m calling my doctor tomorrow
also… is this why my cousin’s face looked like a balloon at her wedding??
😭
Jessie Ann Lambrecht
January 19, 2026 AT 18:57Here’s what nobody’s saying: this isn’t just about drugs. It’s about how we treat patient knowledge.
Most people don’t know how their meds work. They’re handed a script and told ‘take one daily.’ No explanation. No risks. No alternatives.
But when something goes wrong? Suddenly they’re the problem. ‘Why didn’t you tell us?’
That’s not patient responsibility. That’s system failure.
Imagine if every prescription came with a 30-second video: ‘This drug can cause silent swelling. If your lips, tongue, or throat swell - stop it. Call your doctor. Don’t wait. Don’t take Benadryl.’
It’s not hard. It’s not expensive. It’s just… human.
And if you’ve had this reaction? You owe it to others to speak up. Your story might save someone’s life.
I’m getting my medical alert bracelet today.
Ayodeji Williams
January 21, 2026 AT 12:03bro this is all just fear
my uncle took this for 15 years and he’s fine
you people are overreacting
why not just stop taking all meds and live in the jungle
also why is everyone so obsessed with swelling
maybe you just need to chill
and who even has time to read all this
😂