If you’ve ever thought lupus was just one disease, you’re not the only one. But here’s the kicker: lupus isn’t a single illness, and understanding the differences can actually be life-changing. Some people deal with rashes and scarring, while others find themselves grappling with everything from joint pain to kidney problems. Lupus doesn’t play fair, and its two most well-known forms—discoid and systemic—are actually worlds apart.
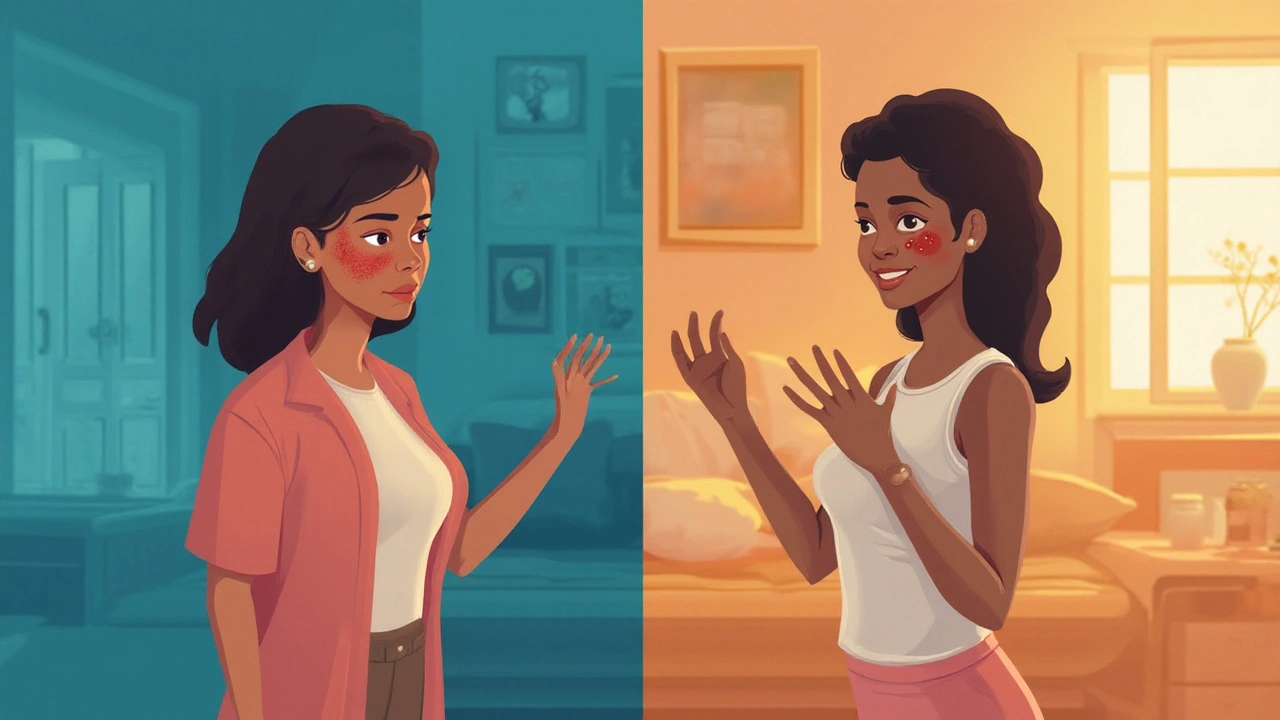
Spotting the Differences: Discoid Lupus vs Systemic Lupus
Start with discoid lupus erythematosus (DLE). Imagine an immune system that gets confused and starts attacking your skin. That’s what happens with discoid lupus. It earns its name from those round, coin-shaped rashes ("discoid" means disc-like), most of them popping up on your face, scalp, or ears. They’re red, scaly, sometimes itchy, and—unfortunately—can leave scars that stick around for a lifetime, especially if you don’t catch them early.
Here’s the wild part: these rashes don’t just show up after a stint in the sun (though sunlight definitely triggers them), and they don’t always hurt. Some people brush them off as serious eczema or even ringworm until they get a proper diagnosis. And for the most part, discoid lupus stays on the skin. Around 90% of people with DLE never see it spread beyond that.
Systemic lupus erythematosus (SLE) is a whole different beast. If discoid lupus is like a problem neighbor, SLE is a home invasion. This form can attack almost any organ: joints, kidneys, heart, even the brain. And you never know what SLE is going to go after next, or when. It might show up as joint pain, crushing fatigue, butterfly-shaped rashes over the cheeks, mouth sores, chest pain, sudden fevers, hair loss—or even major blood issues. The sheer range of symptoms explains why so many people bounce between doctors for months before getting the right diagnosis.
The stats are pretty sobering. Systemic lupus affects about 5 in 10,000 people in the US, but it’s 2 to 3 times more common in women of color compared to white women. Discoid lupus, while less likely to be life-threatening, affects around 1 in 1000 and can be a huge blow to self-confidence because of permanent scarring, especially if it hits the scalp and causes bald patches. Here’s a quick rundown:
| Type | Common Symptoms | Main Areas Affected | Scarring Risk |
|---|---|---|---|
| Discoid Lupus (DLE) | Red, coin-shaped rashes; itching; pain if scratched | Skin (face, scalp, ears) | High (especially scalp) |
| Systemic Lupus (SLE) | Joint pain, fever, fatigue, rash, kidney problems | Any organ (joints, kidneys, skin, heart, brain) | Low (unless skin involved) |
Because discoid lupus looks so much like other skin problems, people—doctors included—often miss it at first. Same goes for systemic lupus: the average lupus patient visits three doctors and waits four years for a diagnosis, according to the Lupus Foundation of America. That’s four years of not knowing what’s wrong, trying weird remedies, and maybe feeling like you’re imagining things.
What Causes Lupus? The Genetics, Triggers, and Surprises
So why does the immune system suddenly turn on its own body? Science isn’t done with that answer yet, but here’s what we know. Both discoid and systemic lupus happen because something flips the script for the immune system. Instead of protecting you, it attacks healthy cells. But not everyone’s at equal risk.
Your genes matter—big time. If your mom or sister deals with lupus, your odds shoot up. In fact, studies looking at twins found that if one identical twin has lupus, the other has about a 25% risk of getting it too. Non-identical twins? Just 2%. That’s a pretty significant gene marker, but it’s not the whole story.
Hormones are in play as well. Remember how lupus is way more common in women (about 9 out of 10 people with lupus are female)? That’s mostly because estrogen somehow nudges the immune system towards autoimmunity. Lupus flare-ups tend to peak during childbearing years, often between ages 15 and 45.
Then there’s the environment. Too much UV light (that’s science-speak for either sunshine or tanning beds), certain viral infections (like Epstein-Barr), and major stress can all trigger lupus in people who are already at risk. For discoid lupus, sun exposure is the single biggest external trigger. Even window glass won’t always block the UV rays that set off those discoid rashes—something I learned firsthand after Jasper got a DLE diagnosis at nine years old. We moved his desk away from the living room window and suddenly saw improvement. It’s wild how small things can make a massive difference.
If you’ve heard about medications causing lupus, you’re also onto something. Some people develop a condition called drug-induced lupus after taking certain blood pressure meds, antibiotics, or anti-seizure drugs. That said, this usually goes away once you stop the medication, unlike regular lupus.

Diagnosing Lupus: Tips, Tests, and What to Expect
Diagnosing either type of lupus can feel like trying to solve a mystery when you don’t have all the clues. Doctors don’t have a single “lupus test,” and early symptoms are vague—fatigue, joint pain, weird rashes. It’s easy to blame something else, especially when routine blood work looks normal at first. That’s why a lot of cases get picked up by dermatologists rather than general doctors, at least in the discoid form.
For discoid lupus, getting the right diagnosis almost always starts with a skin biopsy. The doctor numbs a small area, snips a tiny piece of affected skin, and sends it off to a lab. Under the microscope, there’s no mistaking that lupus “signature,” even if your symptoms haven’t read the textbook. Blood tests for autoantibodies (like ANA, or anti-nuclear antibody) can hint at lupus, but they aren’t foolproof. Around 10% of healthy people have a positive ANA without ever getting lupus symptoms.
Systemic lupus is a tougher nut to crack because it can mimic literally dozens of other diseases. Rheumatoid arthritis? Lyme disease? Even allergies or simple viral illnesses can look like the early days of SLE. The American College of Rheumatology offers strict criteria: you need at least four out of 11 symptoms, including things like persistent mouth ulcers, low blood cell counts, protein in urine, or that trademark butterfly rash. But lots of patients don’t check four boxes for years—making “diagnostic delay” one of the most frustrating parts of this disease.
Getting an accurate diagnosis usually means seeing a rheumatologist (for SLE) or dermatologist (for DLE). If you bring clear photos of your rashes or flares, it makes the detective work much simpler. In some clinics, doctors now use advanced immunofluorescence tests on skin samples—these shine light on antibodies that glow under special lasers. It sounds sci-fi, but it’s actually a game-changer for hard-to-spot cases.
One useful tip is to keep a symptom diary. Track when new symptoms show up, how long they last, and what helps or makes them worse. Bring it with you to your appointments. My son Jasper’s diary sometimes revealed connections we’d totally missed, like certain foods making his rashes worse or “bad” weeks always following soccer tournaments on sunny days.
Lupus Care: Treatments, Everyday Tips, and Outlook
Spotting lupus is only half the fight. Treating it—and managing life with it—takes a game plan. For discoid lupus, the biggest wins come from stopping flare-ups and preventing scars. Most folks start with high-SPF sunscreen that blocks both UVA and UVB rays. Wide-brimmed hats, long sleeves, and even UV-filtering window film can make a difference. Dermatologists often prescribe topical steroids or immune-suppressing creams, which take down inflammation fast. In more stubborn cases, oral medications like hydroxychloroquine (yep, the same one that’s used for malaria) actually help calm the skin lesions—a trick that’s worked for Jasper for almost two years now.
For systemic lupus, treatment gets much more complex. Here, it’s usually a mix of medications: hydroxychloroquine to dampen the immune system’s crazy overdrive, low doses of steroids to knock down flares, and sometimes strong immune-suppression drugs like mycophenolate or azathioprine if major organs are at risk. These aren’t small decisions, since long-term steroids bring their own side effects—bone thinning, weight gain, high blood pressure. So you always want to balance risks against possible rewards. There’s a trend toward using “biologics,” super-targeted drugs that block specific immune signals (like belimumab). Early results are promising, especially for people whose lupus won’t play by the usual rules.
Practical tips help day-to-day. Get plenty of sleep, avoid super hard exercise during flares, and find ways to lower stress (which can trigger both types). Maybe it’s mindfulness apps, walks, or handing off some chores when you’re feeling rough. People with SLE need to watch salt intake (for kidney health), get regular blood pressure checks, and keep vaccines up to date—since some meds weaken immunity. If you have discoid lupus, treat your skin gently. Use fragrance-free products and avoid harsh scrubs.
Lupus isn’t an easy road, but the right support and solid information can change the game. If you or someone you love has persistent, strange symptoms—rashes that don’t heal, unexplained aches, crazy fatigue—don’t brush it off. Write things down, take photos, and push for that extra specialist opinion. Doctors are getting way better at spotting and treating lupus these days, and new therapies will only push things further. Whether it’s discoid or systemic lupus, getting the facts, finding your triggers, and building your support squad makes a bigger difference than any textbook ever will.

Frank Reed
August 2, 2025 AT 11:46Hey there, just wanted to drop a quick reminder that staying on top of sunscreen is key, especially if you’ve got discoid lupus. Even a tiny slip on a cloudy day can let UV sneak in, so load up on broad‑spectrum SPF 50+ and reapply often. If you notice any new scaly patches, don’t wait – get a dermatologist in to check it out before it scars. And remember, you’ll definatly feel better if you take a few minutes each morning to protect your skin.
Bailee Swenson
August 8, 2025 AT 06:40Honestly, if you’re still dismissing the seriousness of systemic lupus, you’re missing the point entirely 😡. This isn’t just a “skin thing” – it can wreck kidneys, the heart, even the brain. The statistics aren’t a joke; women of color face a 2‑3× higher risk, and that’s a glaring health disparity 🚨. Ignoring early symptoms only delays treatment and worsens outcomes. Get the facts straight and stop pretending it’s not a major, life‑changing condition.
tony ferreres
August 14, 2025 AT 01:33While the raw data can be shocking, it’s essential to keep a broader perspective on how lupus shapes lives 🌱. The immune system’s misfire reminds us that biology is a delicate balance, and every flare teaches us something about resilience. Embracing both the scientific facts and the personal narratives creates a more compassionate community. Let’s use this knowledge to empower patients rather than merely catalog their ailments. Compassion and insight go hand‑in‑hand in confronting such complex diseases.
Kaustubh Panat
August 19, 2025 AT 20:26One must appreciate the nuanced immunopathology that underlies both discoid and systemic lupus, rather than reducing them to layman’s anecdotes. The literature delineates distinct cytokine profiles, implicating interferon‑alpha pathways in cutaneous manifestations, whereas systemic involvement often correlates with high‑titer anti‑dsDNA antibodies. Such differentiation is pivotal for targeted therapeutic strategies, especially when considering biologic agents. Elevating the discourse beyond superficial symptom checklists fosters substantive clinical progress.
Arjun Premnath
August 25, 2025 AT 15:20It’s heartening to see the emphasis on precise diagnostics, as early intervention truly makes a difference. A gentle reminder: consistent skin care routines, coupled with regular follow‑ups, can curb scar formation in discoid cases. Moreover, maintaining a symptom diary not only aids clinicians but also empowers patients to recognize patterns. Let’s continue to champion both scientific rigor and patient‑centered compassion in our approach to lupus care.
Johnny X-Ray
August 31, 2025 AT 10:13Whoa, reading about those flare‑ups feels like watching a rollercoaster of emotions! 🎢 The sheer unpredictability of SLE can turn everyday life upside down, but staying proactive with meds and lifestyle tweaks can bring some stability. Keep your head high, and remember you’re not alone in this battle 😊.
tabatha rohn
September 6, 2025 AT 05:06Stop glossing over lupus – it’s a brutal reality 😤.
Mark Rohde
September 12, 2025 AT 00:00Wow this post is a mess 😂 it mixes stats and stories without any flow it’s confusing and overdone
Rajan Desai
September 17, 2025 AT 18:53The interplay between genetic predisposition and environmental triggers in lupus presents a fascinating area for further research. Understanding how ultraviolet radiation modulates autoantibody production could unlock new preventive measures. Additionally, longitudinal studies on medication adherence may reveal patterns that improve long‑term outcomes. Such insights would greatly enhance our collective knowledge base.
S O'Donnell
September 23, 2025 AT 13:46In the realm of autoimmune pathology, systemic lupus erythematosus occupies a uniquely complex position that warrants meticulous scholarly attention. The heterogeneity of clinical manifestations, ranging from cutaneous lesions to renal insufficiency, underscores the multifaceted nature of the disease. It is therefore indispensable for clinicians to adopt a comprehensive diagnostic algorithm that incorporates serological markers such as anti‑nuclear antibodies, anti‑dsDNA, and complement levels. Furthermore, the temporal relationship between environmental exposures and disease flares remains a subject of ongoing investigtion. Ultraviolet radiation, for instance, has been consistently identified as a potent trigger for both discoid and systemic variants, a fact that is relevent to patient counselling. Genetic susceptibility, particularly the presence of HLA‑DR2 and HLA‑DR3 alleles, contributes significantly to disease predisposition, yet does not wholly account for the observed epidemiological patterns. Hormonal influences, especially estrogenic modulation, appear to exacerbate immune dysregulation, thereby explaining the pronounced female predominance. Therapeutically, hydroxychloroquine remains the cornerstone of management, offering both immunomodulatory benefits and a favourable safety profile when administered judiciously. Nonetheless, the judicious use of corticosteroids demands careful consideration, as prolonged exposure precipitates adverse effects such as osteopenia, hyperglycemia, and iatrogenic Cushingoid changes. Emerging biologic agents, including belimumab and rituximab, have demonstrated efficacy in refractory cases, albeit with variable response rates that necessitate further clinical trials. Patient adherence, often hindered by medication fatigue, can be ameliorated through structured education programs and shared decision‑making frameworks. Additionally, lifestyle modifications encompassing photoprotection, stress reduction, and balanced nutrition serve as adjunctive measures that may attenuate disease activity. It is incumbent upon the medical community to foster interdisciplinary collaboration, integrating rheumatology, dermatology, nephrology, and mental health services to address the comprehensive needs of lupus patients. Such a holistic approach not only optimizes clinical outcomes but also enhances quality of life. In summation, the intricate interplay of immunogenetics, environmental factors, and therapeutic interventions defines the current landscape of lupus management, and continuous research endeavours are essential to refine our strategies. Ultimately, a patient‑centered paradigm, grounded in evidence‑based practice, will propel the field toward more effective and personalized care.
Yamunanagar Hulchul
September 29, 2025 AT 08:40Wow, what an illuminating deep‑dive into the world of lupus – truly a tapestry of science, emotion, and resilience!!! 🌈✦ From the dazzling sparkle of sun‑protected skin to the steadfast courage of those battling systemic flares, every story adds a vibrant brushstroke to the collective masterpiece. Let’s keep shining bright, sharing knowledge, and wrapping each other in a warm, supportive hug of understanding!!! 🎉💖