Anticholinergic Burden Calculator
Medication List
Add all medications you take (prescription, OTC, herbal)
Your Total Score
Score ≥ 3: 54% higher dementia risk over 7 years
Medication List
Risk Assessment
Score 0-2: Low risk of cognitive decline. Monitor for side effects.
Score 3-4: Moderate risk. Consider alternatives with lower anticholinergic burden.
Score 5+: High risk. Consult your doctor immediately about reducing burden.
When you take a tricyclic antidepressant like amitriptyline or nortriptyline for depression or nerve pain, you might not realize you’re also loading your body with a hidden risk - one that can cloud your memory, slow your thinking, and even mess with your heart rhythm. These drugs work by boosting serotonin and norepinephrine, but they also block acetylcholine, a key brain chemical that helps with attention, memory, and muscle control. This blocking effect is called anticholinergic burden, and it’s not just a side effect - it’s a measurable, serious threat, especially for people over 50.
What Is Anticholinergic Burden?
Anticholinergic burden isn’t about one drug. It’s the total amount of anticholinergic activity your body gets from everything you take - prescriptions, over-the-counter sleep aids, allergy meds, even bladder pills. Think of it like a scorecard. The Anticholinergic Cognitive Burden (ACB) Scale rates drugs from 1 to 3:- ACB 1 = possible anticholinergic effect
- ACB 2 = moderate effect
- ACB 3 = strong, definite effect
How TCAs Blur the Line Between Depression and Dementia
Many older adults start taking TCAs for depression or chronic pain. But then they begin forgetting names, losing track of conversations, or struggling to find the right words. Their family worries - is this Alzheimer’s? The doctor orders a scan. But here’s the catch: these symptoms aren’t always from brain degeneration. They’re from the drug. Clinicians across the UK and US report cases where patients on amitriptyline were mistakenly diagnosed with early dementia. Their memory improved within months after stopping the drug. Dr. Helga Bennett, cited in NHS Somerset guidelines, puts it plainly: “The presence of a substantial anticholinergic burden may mimic the symptoms of dementia and therefore lead to a false diagnosis.” This isn’t rare. A 2022 survey by the National Council on Aging found that 68% of patients over 65 taking TCAs had at least two anticholinergic side effects - dry mouth, constipation, blurred vision, urinary retention - and 32% said their memory problems were bad enough to consider quitting. These aren’t just inconveniences. They’re warning signs that your brain is being chemically fogged.The Hidden Heart Risk: More Than Just Dizziness
While memory loss grabs headlines, the cardiac dangers of TCAs are just as serious - and often overlooked. These drugs act like class 1A antiarrhythmics, meaning they slow down the heart’s electrical signals. At therapeutic doses, amitriptyline can prolong the QRS complex by 10-25%. In overdose, that jumps to 50%. Even worse, it prolongs the QT interval, which can trigger dangerous heart rhythms like torsades de pointes. Studies show TCAs carry about three times the risk of arrhythmias compared to SSRIs like sertraline. Amitriptyline specifically raises the risk of QT prolongation by 2.8 times compared to sertraline. For someone with existing heart disease, high blood pressure, or a history of fainting, this isn’t a gamble - it’s a countdown. One patient in a Mended Hearts support group described how, after just three weeks on amitriptyline for depression, he developed palpitations and dizziness. He ended up in the ER, where doctors found significant QT prolongation. He was taken off the drug immediately. His story isn’t unique. Cardiologists now routinely check ECGs before prescribing TCAs - especially in people over 60.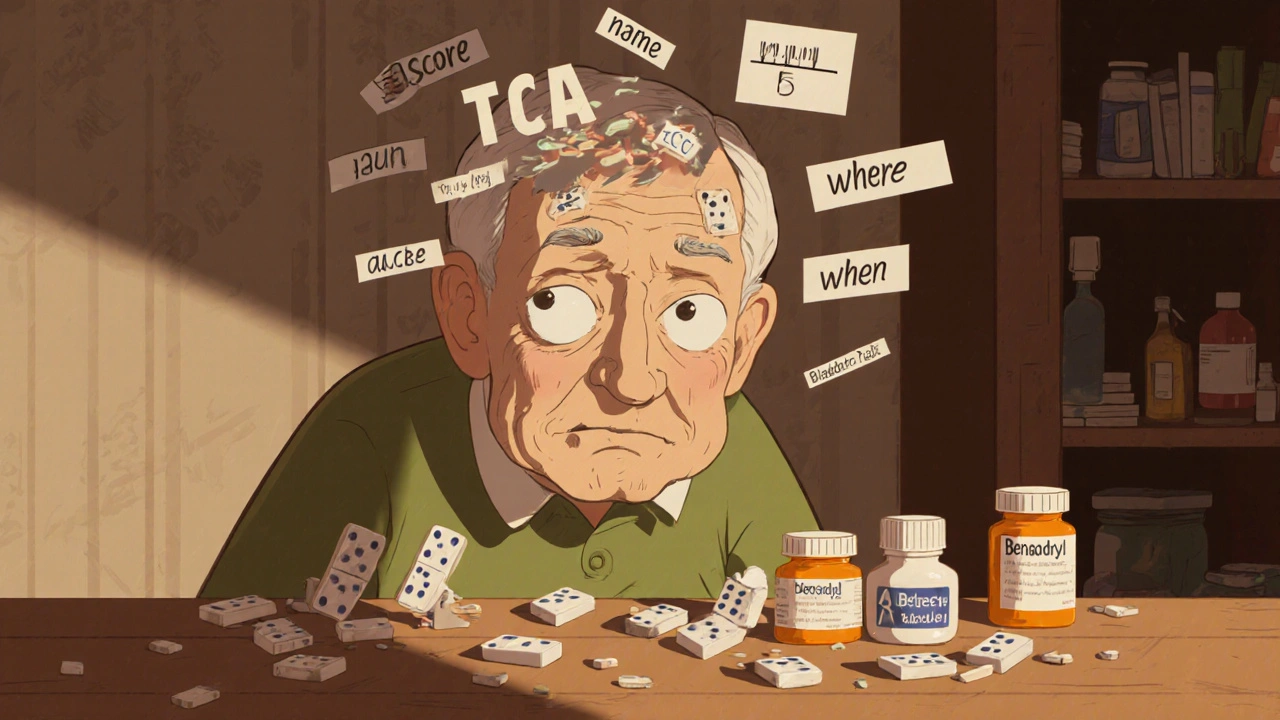
Why TCAs Are Still Prescribed - and When They Might Still Make Sense
You might wonder: if the risks are this high, why are doctors still writing these prescriptions? The answer is simple - they work. For some people with treatment-resistant depression, or severe neuropathic pain that hasn’t responded to anything else, TCAs can be a lifeline. But here’s the key: they’re a last resort. Modern antidepressants like SSRIs (sertraline, escitalopram) and SNRIs (duloxetine, venlafaxine) have ACB scores of 0 or 1. They’re just as effective for most types of depression - with far fewer side effects. Duloxetine, for example, is just as good for nerve pain as amitriptyline, but doesn’t carry the same brain or heart risks. The National Institute for Health and Care Excellence (NICE) guideline NG97 says clearly: “Minimise the use of medicines associated with increased anticholinergic burden.” The Beers Criteria, used by doctors in the US and UK, lists TCAs as potentially inappropriate for adults over 65 - unless other options have failed and the benefits clearly outweigh the risks.What to Do If You’re Taking a TCA
If you’re on amitriptyline, nortriptyline, or another TCA, don’t stop cold turkey. Withdrawal can cause nausea, anxiety, and even rebound depression. Instead, talk to your doctor about a safe plan. Here’s what to ask for:- Calculate your total ACB score - include every pill, even OTC ones like Nytol or Piriton.
- Ask if your current dose is the lowest possible for your condition.
- Request a trial of switching to an SSRI or SNRI - many patients do just as well, or better.
- Get an ECG if you’re over 50 or have heart issues.
- Ask about non-drug options: CBT for depression, physical therapy or acupuncture for pain.

The Bigger Picture: Why This Matters Now
Prescribing of TCAs has already dropped sharply. In the US, they made up 15% of antidepressant prescriptions in 2000. By 2020, that was down to 4.7%. New antidepressants approved since 2010 are almost all low-anticholinergic. The market is moving away from TCAs - and for good reason. AI tools are now being tested in UK hospitals to automatically flag high ACB scores during e-prescribing. NHS Digital is piloting systems that warn doctors before they write a prescription that pushes a patient’s total ACB score above 3. The message is clear: anticholinergic burden isn’t a footnote. It’s a red flag. And for tricyclic antidepressants, that flag is bright red - with no gray area.Alternatives That Work Without the Risk
You don’t have to suffer through dry mouth and brain fog to treat depression or pain. Here are safer, evidence-backed options:- SSRIs (sertraline, escitalopram): ACB 0-1. First-line for depression. Minimal cardiac risk.
- SNRIs (duloxetine, venlafaxine): ACB 0-1. Also effective for nerve pain - often better than TCAs.
- CBT (Cognitive Behavioral Therapy): Proven for depression and chronic pain. No drugs needed.
- Pregabalin or gabapentin: For neuropathic pain. No anticholinergic effect.
- Topical capsaicin or lidocaine patches: For localized nerve pain.
Do tricyclic antidepressants cause dementia?
Tricyclic antidepressants don’t directly cause dementia, but they significantly increase the risk of developing it. Long-term use of drugs with high anticholinergic burden - like amitriptyline or nortriptyline - is linked to a 54% higher chance of dementia over seven years. In many cases, the cognitive symptoms they cause mimic dementia and can be mistaken for it. These effects may not fully reverse even after stopping the drug.
Is amitriptyline safe for older adults?
Amitriptyline is generally not considered safe for older adults. It has the highest possible anticholinergic burden (ACB=3) and carries a high risk of cognitive decline, falls, urinary retention, and dangerous heart rhythm changes. Guidelines from NICE and the Beers Criteria recommend avoiding it in people over 65 unless other treatments have failed and the benefits clearly outweigh the risks.
Can I stop taking a TCA on my own?
No. Stopping tricyclic antidepressants suddenly can cause withdrawal symptoms like nausea, anxiety, insomnia, and worsening depression. Always work with your doctor to create a slow tapering plan - usually over 4 to 8 weeks. Your doctor can also help you switch to a safer alternative like an SSRI or SNRI.
What medications add to anticholinergic burden?
Many common medications contribute, including over-the-counter sleep aids (diphenhydramine/Nytol), allergy pills (chlorphenamine/Piriton), bladder control drugs (oxybutynin), and some motion sickness tablets. Even one of these combined with a TCA can push your total ACB score into the danger zone (3 or higher).
Are there tests to check for anticholinergic burden?
Yes. The Anticholinergic Cognitive Burden (ACB) Scale is the most widely used tool. Doctors can calculate your total score by adding up the ACB ratings of every medication you take. Many UK electronic health systems now have built-in ACB calculators that flag high-risk prescriptions automatically. You can also ask your pharmacist to review your full list of meds.


Doug Pikul
October 31, 2025 AT 04:45Doctors need to stop treating seniors like walking pill dispensers.
Craig Venn
November 1, 2025 AT 02:46Christine Mae Raquid
November 2, 2025 AT 07:58Alicia Buchter
November 2, 2025 AT 22:55Dave Collins
November 4, 2025 AT 06:32Idolla Leboeuf
November 6, 2025 AT 02:57Zach Harrison
November 6, 2025 AT 06:46Matthew Williams
November 7, 2025 AT 09:28Terri-Anne Whitehouse
November 8, 2025 AT 09:21Sue Ausderau
November 9, 2025 AT 21:49Cole Brown
November 11, 2025 AT 09:01MaKayla VanMeter
November 11, 2025 AT 23:15M. Kyle Moseby
November 13, 2025 AT 08:50